- Visibility 241 Views
- Downloads 81 Downloads
- Permissions
- DOI 10.18231/j.jdp.2022.038
-
CrossMark
- Citation
Grinspan’s span syndrome – A case report of a triad
- Author Details:
-
Bilal Jawhar Ghazi *
-
C Ganesh
Abstract
Oral Lichen Planus (OLP) is chronic autoimmune mucocutaneous inflammatory condition affecting the oral cavity and the skin but it is been said OLP is also associated with other systemic diseases specifically hypertension and diabetes mellitus the triad (OLP, hypertension, diabetes mellitus) is known as Grinspan’s Syndrome. Since its inception has been an arena of interest. It has appeared very lucrative to many researchers as it lacks clarity and enhanced ambiguity. This article, we present a case of 46 year old female patient with a complaint of white patch and burning sensation which have been histologically proven case of oral erosive lichen planus and patient also had a positive history of hypertension and diabetes mellitus. Malignant transformation is the most significant complication of long standing and non healing Lichen Planus. Repeated follow up and biopsies are mandatory for prevention and early detection of malignant transformation.
Key Messages: In this article we are presenting a case report of Grinspan’s Syndrome which is a triad of oral erosive lichen planus, diabetics and hypertension and a review of literature on possible reason why the triad of above mentioned diseases is occurring together in patients.
Introduction
Lichen Planus was initially described by a British physician Wilson Erasmus in the year 1869. It is an autoimmune condition manifested on the skin, hair, eyes, mucous membranes, and nails.[1], [2], [3] Those lesions which are present in the oral cavity are referred as oral lichen planus (OLP). Across worldwide among general population, OLP prevalence is about 0.5–2% with females predilection.[4] A cross sectional study done among tribal and suburban population of Maharashtra incidence of grinspan syndrome was found to be 1.62%, mainly seen in sub-urban females of 35-50 years.[5] Around 53.6% of cutaneous LP patients are associated with OLP.[6] Nowadays, Both cutaneous form and oral lichen planus are identified as a chronic muco-cutaneous inflammatory condition which arises from the stratified squamous epithelium. Grinspan et al in 1964, at first reported the prevalence of coexistence of the traid of OLP, diabetes mellitus and hypertension at the Fifth Latin American Dermatology Congress. Later in 1965, Jolly, Powell, Howell and Rick supported the existence of this symptomatic triad.[7] In this article, we present a case of symptomatic erosive oral lichen planus with a history of vascular hypertension along with which, diabetes mellitus type II was diagnosed. The co-existence of all three together confirms the case as Grin’s span syndrome.
Case History
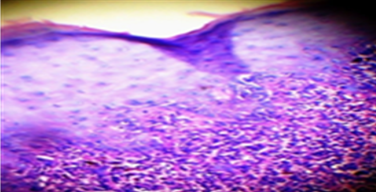
A 46-year-old female patient had come to oral medicine department with the chief complaint of white patches and burning sensation present for past 5 months. The patient history revealed that she had hypertension for a duration of 1 years and under medication for past 6 months amlong (amlodipine) 5 mg. General examination revealed that she had recent loss of weight and excessive thrust for past 4 months. No. other relevant family /personal history. Intra-oral examination revealed, a radiating grayish white lines on the right side ([Figure 1]) and left side of buccal mucosa ([Figure 2]) along with areas gingival desquamation was observed in the gingiva ([Figure 3]). After correlating history & clinical examination, gave a differential diagnosis of oral Lichen Planus and lichinoid reaction. On biochemical and haematological investigation, fasting blood glucose level was found to be 170mg/dl, post prandial blood glucose was 485mg/dl and her HbA1c was 9. Incisional biopsy was done from the right side of buccal mucosa and histopathalogical section of ulceration revealed sub epithelial band of lymphocytic infiltrate, irregular thickening of the epidermis and elongation of the rete ridges with hyperkeratosis and degeneration of basement membrane ([Figure 4]) which confirmed the diagnosis of oral erosive lichen planus. Type II diabetes mellitus was finally confirmed based on the results of biochemical and haematological investigation.



On correlating the triad of hypertension, lichen planus and diabetes, the case was finally diagnosed as Grinspan’s syndrome. She was referred to general physician for management of diabetes mellitus for which she was prescribed medications. Oral lesions are treated with Kenacort 0.1% Oral Paste (triamcinolone acetonide 0.1% in aqueous solution), 3 times daily for more than a month. Patient reviewed after 1 month, patient was found to be having a complete relief of burning sensation symptom and white patches did not increase or decrease in size it remains unchanged.
Discussion
Lichen planus has a multifactorial etiology. It is an auto immune disorder which is T cell mediated. The primary event in occurrence of OLP and the factors which influence the susceptibility are not known. Some state a predisposing genetic factor coupled with other factors including, emotional stress, drug induced hypersensitivity, hypersensitivity reactions to dental filling materials, food, etc. OLP has a variable clinical presentation. OLP is of six subtypes namely; reticular, popular, plaque like, erosive, atrophic and bullous. The most prevalent form is the reticular OLP in which Whick-ham striae, an asymptomatic white lace type pattern is seen on the cheek or buccal mucosa.[8] Typical lesions of OLP are bilateral in occurrence with posterior buccal mucosa being the most common site. However, it can also be seen tongue, gingiva, retromolar/tuberosity region, vestibule, floor of the mouth and lips. In our case, predominantly gingiva was affected causing desquamation and also buccal mucosa bilaterally. In spite of OLP lesions having distinct clinical presentations, under rare circumstances, a confusing array of patterns may be observed.
A range of 10% - 85% prevalence of DM in OLP patients has been reported.[9], [10] Studies state that endocrine dysfunction in DM may lead to an immunological defect, which can result in formation of OLP. A total of 3 cases with apparent drug induced Grinspan’s syndrome with a triad of Oral Lichen Planus, diabetes mellitus and hypertension are reported.[11] OLP has been reported in many cases with medical history of diabetes due to the pathogenesis occurring in diabetic patients. Because drugs used to treat hypertenstion and diabetes mellitus may also cause lichenoid type of reaction in the oral cavity, lichenoid reaction causes lesions in the oral cavity which is similar to that of lichen planus hence the name is substantiated as lichenoid reactions, therefore a different hypotheses is put forth Grinspan’s syndrome may be drug induced phenomenon but thankfully gold standard biopsy help to distinguish (iatrogenic) lichenoid reaction from OLP.[12]
Whereas, this case showed sub epithelial band of lymphocytic infiltrate, irregular thickening of the epidermis and elongation of the rete ridges with hyperkeratosis and degeneration of basement membrane (Fig 4) which confirmed the diagnosis of erosive OLP. Another useful aid in the differentiation of lichenoid and OPL is examination under Immunofluorescent. Gold standard in treatment of OLP is topical and systemic corticosteroids but literature also showed evidence of systemic and topically administered all-trans retinoic acid, Vitamin A, systemic etretinate, and systemic and topical isotretinoin is very effective in the treatment of OLP,[13] cyclosporine and photodynamic therapy are some of the other treatment modalities. In our case, we have treated with Kenacort 0.1% Oral Paste (triamcinolone acetonide 0.1% in aqueous solution) along with supplement therapy with vitamins and patient was regularly reviewed after 1 week, and symptoms relieved with medication after1month period.
Grinspan’s syndrome should always be suspected in patients with proven OLP with a history of hypertension, diabetes mellitus. Finally, conclude by quoting the words of William Osler “Mouth is the mirror of the body” oral lesions may have connection with systemic diseases, this case Grins span syndrome is one such finding were oral erosive lichen planus is connected with systemic illness of hypertension and diabetes mellitus.
Acknowledgement
Dr. Divya VC, Reader, Department of Oral Medicine and Radiology, SRM Kattankulathur Dental College and Hospital, SRM Institute of Science and Technology, SRM Nagar, Kattankulathur, 603203, Kanchipuram, Chennai, Tamil Nadu, India
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
None declared.
References
- Pandhi D, Singal A, Bhattacharya SN. Lichen planus in childhood: A series of 316 patients. Pediatr Dermatol. 2014;31(1):59-67. [Google Scholar] [Crossref]
- Pakravan M, Klesert T, Akpek E. Isolated lichen planus of the conjunctiva. Br J Ophthalmol. 2006;90(10):1325-6. [Google Scholar] [Crossref]
- Canto H, Müller A, Sérgio P. Oral lichen planus (OLP): clinical and complementary diagnosis. An Bras Dermatol. 2010;85(5):669-75. [Google Scholar] [Crossref]
- Laeijendecker R, Joost TV, Kuizinga M, Tank B, Neumann HM. Premalignant nature of oral lichen planus. Acta Derm Venereol. 2005;85(6):516-20. [Google Scholar] [Crossref]
- Lalitkumar P, Snehal D, Kiran S, SC, MM, VK. Incidence of grinspan syndrome among tribal and suburban population of Maharashtra - A cross sectional study. Indian J Dent Res. 2021;32(1):115-9. [Google Scholar] [Crossref]
- Cassol-Spanemberg J, Blanco-Carrión A, Rivera-Campillo MR, Estrugo-Devesa A, Jané-Salas E, López-López J. Cutaneous, genital and oral lichen planus: A descriptive study of 274 patients. Med Oral Patol Oral Cir Bucal. 2019;24(1). [Google Scholar]
- Colella G, Itro A, Grovo G. [A case of a carcinoma arising in lichen planus in a subject with diabetes mellitus and arterial hypertension (Grinspan's syndrome)]. Minerva Stomatol. 1992;41(9):417-20. [Google Scholar]
- Gupta S, Jawanda M. Oral Lichen Planus: An Update on Etiology, Patho-genesis, Clinical Presentation, Diagnosis and Management. Indian J Dermatol. 2015;60(3):222-9. [Google Scholar]
- Howell F, Rick G. Oral lichen planus and diabetes: A potential syndrome. J Calif Dent Assoc. 1973;1(1):58-9. [Google Scholar]
- Lundström I. Incidence of diabetes mellitus in patients with oral lichen planus. Int J Oral Surg. 1983;12(3):147-52. [Google Scholar] [Crossref]
- Lamey P, Gibson J, Barclay S, Miller S. Grinspan's syndrome: a drug-induced phenomenon?. Oral Surg Oral Med Oral Pathol. 1990;70(2):184-5. [Google Scholar] [Crossref]
- Haute VVD, Antoine J, Lachapelle J. Histopathological discriminant criteria between lichenoid drug eruption and idiopathic lichen planus: retrospective study on selected samples. Dermatologica. 1989;179(1):10-3. [Google Scholar]
- Eisen D. The clinical manifestations and treatment of oral lichen planus. Dermatol Clin. 2003;21(1):79-89. [Google Scholar]
How to Cite This Article
Vancouver
Ghazi BJ, Ganesh C. Grinspan’s span syndrome – A case report of a triad [Internet]. J Dent Panacea. 2022 [cited 2025 Sep 29];4(4):179-182. Available from: https://doi.org/10.18231/j.jdp.2022.038
APA
Ghazi, B. J., Ganesh, C. (2022). Grinspan’s span syndrome – A case report of a triad. J Dent Panacea, 4(4), 179-182. https://doi.org/10.18231/j.jdp.2022.038
MLA
Ghazi, Bilal Jawhar, Ganesh, C. "Grinspan’s span syndrome – A case report of a triad." J Dent Panacea, vol. 4, no. 4, 2022, pp. 179-182. https://doi.org/10.18231/j.jdp.2022.038
Chicago
Ghazi, B. J., Ganesh, C.. "Grinspan’s span syndrome – A case report of a triad." J Dent Panacea 4, no. 4 (2022): 179-182. https://doi.org/10.18231/j.jdp.2022.038
