- Visibility 15 Views
- Downloads 2 Downloads
- DOI 10.18231/j.jdp.2024.038
-
CrossMark
- Citation
Efficacy of vibrotactile device Dentalvibe in the assessment of pain during local anaesthesia in pediatric dental patients in comparison to conventional techniques: A comparative clinical study
- Author Details:
-
Gaurav Gupta *
-
D K Gupta
-
Priyanka Gupta
-
Parth Shah
-
Neeraj Chandra
-
Kuldeep Singh Rana
Introduction
In July 2020, the International Association for the Study of Pain declared a revision to the concept of pain. The verbal description was one of the expressive actions used to characterize pain, defined as a subjective experience impacted by biological, psychological, and social elements. [1], [2]
In a pediatric dentistry clinic, good behaviour guidance is based on effective pain management.[3]
Three controlled studies on needle less devices have been reported. In a trial, the needle less approach (INJEX) appeared to offer faster anaesthetic outcomes, although the difference was not significant.[4]
The development of a computer-controlled local anaesthetic delivery system (CCLAD) aims to lessen the discomfort that comes with administering local anaesthetic injections. The flow of a local anaesthetic solution is controlled by a pressure-activated foot control pedal.[5]
The purpose of our study was to compare the pain perception and patient comfort between the use of a dentalvibe, conventional cartridge syringe, CCLAD, topical jelly, and NIOS in children requiring local anaesthesia for routine oral surgical procedures via a VAS 10-point scale.
Materials and Methods
Study type: This comparative, split-mouth, randomized controlled clinical study was carried out in a private dental clinic for the duration of 6 months.
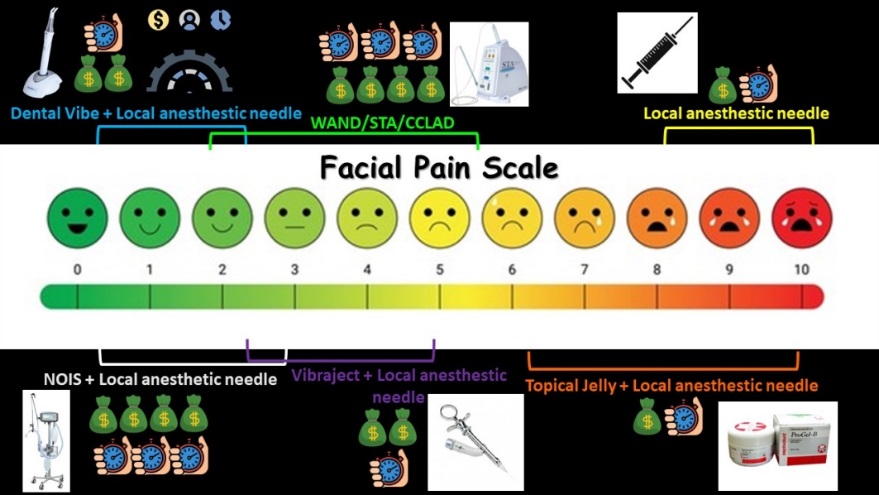
Sample selection: Overall, 200 patients (boys and girls) were screened out of which 150 were selected based on inclusion criteria and were randomly divided into 6 test groups: Group A (DentalVibe+ Local anaesthetic needle), Group B (NIOS+ Local anaesthetic needle), Group C (WAND/STA/CCLAD), Group D (Vibraject + Local anaesthetic needle), Group E (Topical jelly+ local anaesthetic needle), Group F(Local anaesthetic needle).
Inclusion criteria
Children 8–12 years of age.
Positive or definitely positive behaviour according to the Frankl scale.
Children who needed dental chair treatment and those in need of general anaesthesia were excluded from the study.
Free from allergies to the topical anaesthetic used in the study.
Parent consent for child’s participation.
There are no neurological or psychiatric abnormalities in the child.
Intervention and monitoring: Allocated patients in each group; before the commencement of the procedure, the use of the visual analog scale (VAS) was explained. All techniques employed identical 30-gauge, 1.5-inch-long needles and, 1.8-ml Septodont® cartridges to minimize the chance of confounding variables.
Every group received infiltration with a local anaesthetic injection, which comprised the administration of 1.8 ml of 2% lidocaine along with 1: 100,000 adrenaline (Xylocaine, Dentsply, PA, USA) respectively. With Dental Vibe in Group A; device tip is placed in the mucosa and activated for 5 seconds, and the needle is inserted as close to the prong while the vibration is still on after anaesthetic infiltration device is kept on for 5 more seconds. Group B with NIOS, Group C with CCLAD via (WAND, Milestone Dental, CA, USA) as per manufacturer recommendations, Group D ( Vibraject + Local anaesthetic needle), topically anaesthetized with 20% benzocaine gel for 1 minute (GINGICaine, Belport County, CA, USA) in Group E, and conventional cartridge syringe in Group F.
After the injection, the patients were asked to rate their pain on a scale of 10, with 1 being the least painful and 10 being unbearable pain.
Statistical analysis
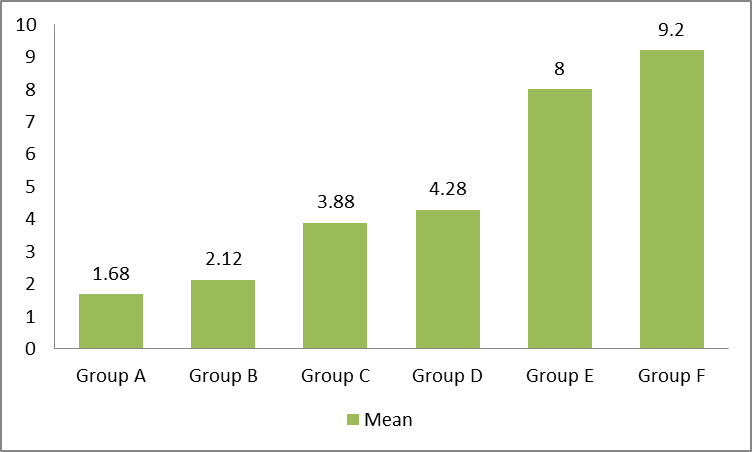
Statistical analysis was conducted using tools of descriptive statistics, such as means for representing quantitative data. The VAS's mean pain scores, which are represented by numerical symbols, will be compared. Each group had 25 individuals. The resultant sum value for 10 point scale for each group was calculated, and the mean was taken as follows ([Figure 1]):
Mean=Σxin
x̄ is the sample mean
– xi represents each data point in the dataset
– ∑(xi) is the sum of all data points
– n is the total number of data points
Pain scale range:
0-2 Mild
3-5 Moderate
6-7 Severe
7-8 Very Severe
9-10 Worst pain
Results
Sum of each data set ([Table 1]):
|
Group |
Sum |
|
A |
42 |
|
B |
53 |
|
C |
97 |
|
D |
107 |
|
E |
200 |
|
F |
230 |
Mean value for each group ([Table 2]):
|
Group |
Mean |
|
A |
1.68 |
|
B |
2.12 |
|
C |
3.88 |
|
D |
4.38 |
|
E |
8 |
|
F |
9.2 |
The calculative mean obtained represented Group A had least mean of pain whereas Group F has highest pain assessment value. ([Figure 2])
Least pain was analysed in Dentalvibe and NIOS whereas for all other techniques pain was from moderate to severe and worst pain was found in case of conventional needle technique.([Figure 3])
Discussion
Local anaesthesia is the backbone of pain control and is essential for a pain-free dental practice. However, local anaesthetic injections are still one of the most anxiety-inducing procedures, especially in paediatrics. [6]
Most dental and oral surgical procedures are performed under local anaesthesia; therefore, failure to properly assess and control pain can lead to problems such as elevated blood pressure, vasovagal reflexes, and treatment interruptions. [7], [8]
Moreover, there isn't a gold standard for diagnosing sudden tooth discomfort. As a result, it is required to create more precise assessment methods for measuring acute pain in dentistry. [9]
The effectiveness of the DV device is examined in this study in a sophisticated way using both subjective and objective assessments of dental fear, anxiety, pain, and heart rate. This is because the subjective assessment of pain by pediatric patients may have an impact on the dependability of the results.
Pain following an LA injection is associated with the needle's entry as well as the tension produced by the tissue expanding during the anaesthetic’s infiltration. In addition to reducing needle prick pain, the DV's vibration may lessen infiltration discomfort by physically aiding in the anaesthetic fluid's dispersion. Although it is hypothesized that it might promote anaesthetic effect induction, a study by Shaefer et al. found that the use of DV did not influence the time for complete anaesthesia (p>0.05). [10] In research, there are few studies regarding the use of vibrotactile devices in pediatric patients. [11], [12] According to the findings of several research, DV can help juvenile patients cope with the pain of dental injections.[13], [14] To date, several pharmaceutical therapies, such as topical anaesthetics, physical techniques, such as cold and acupuncture or gadgets, and psychological interventions, such as distraction strategies, have been evaluated for their ability to reduce pain in pediatric patients during needle-related operations. [15]Recently, vibrating devices have been used successfully to distract pediatric patients and mask the pain of intramuscular injections and venepuncture. [16]
This study used a parallel-arm randomized controlled clinical trial design to evaluate the effectiveness of a vibrating device in lowering pain and anxiety in children receiving maxillary local infiltration anaesthetic. According to our findings, the experimental tool had a statistically significant impact on lowering procedural pain as reported by the patient, procedural pain and anxiety as reported by observers, and procedural pain and anxiety as reported by parents during dental anaesthesia-related operations. These outcomes support the findings of earlier research. [17] Reporting the success with the combined use of cold and vibration to alleviate discomfort and fear in children undergoing maxillary infiltration dental anaesthesia. During dental operations, the experimental vibration gadget can lessen oral pain. Therefore, it could be considered a valuable help for clinicians, together with other new improvements that have been demonstrated to reduce oral discomfort, such as digital impressions. [18]
The findings of this study have a significant clinical application in the field of dentistry and are consistent with prior research demonstrating the advantages of vibration devices in reducing pain during other invasive dental procedures. The results of this study demonstrated the effectiveness of vibrating devices in reducing injection-related pain, but the authors feel that additional strategies, such as patient education and incentives, should be used to further minimize discomfort.
The inclusion of only cooperative youngsters, who make up the majority of pediatric patients in dental practice, was one of our study's primary drawbacks.
However, the findings of our research cannot be generalized to children displaying disruptive behaviour in the dental office.
Limitations
Limited sample size with several groups and age ranges.
Conclusion
The experimental device appears to be a simple, practical, and non-invasive way to give pediatric dental anaesthesia. The authors conclude that giving children an external vibration application can greatly lessen the pain they feel during an oral anaesthetic injection. Particularly for young children, more study is needed to evaluate the effectiveness of this method for different intraoral sites and local dental anaesthetic approaches. This might be done with a larger sample size and include parental pain ratings as well.
Source of Funding
None.
Conflict of Interest
None.
References
- . International Association for the Study of Pain. IASP announces revised definition of pain. 2023. [Google Scholar]
- SN Raja, DB Carr, M Cohen, NB Finnerup, H Flor, S Gibson. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 2020. [Google Scholar]
- M Ashkenazi, S Blumer, I Eli. Effectiveness of computerized delivery of intrasulcular anesthetic in primary molars. J Am Dent Assoc 2005. [Google Scholar]
- G Saleh, Wh-M Raab. Efficiency of a needle-free injector-system for dental local anesthesia. J Dent Res 2002. [Google Scholar]
- EJ Kwak, NS Pang, JH Cho, BY Jung, KD Kim, W Park. Computer-controlled local anesthetic delivery for painless anesthesia: a literature review. J Dent Anesth Pain Med 2016. [Google Scholar]
- B Deacon, J Abramowitz. Fear of needles and vasovagal reactions among phlebotomy patients. J Anxiety Disord 2006. [Google Scholar]
- AN Jadhav, PR Tarte. Acute cardiovascular complications in patients with diabetes and hypertension: management consideration for minor oral surgery. J Korean Assoc Oral Maxillofac Surg 2019. [Google Scholar]
- H Shimoda, T Takahashi. Intravenous sedation management for an outpatient with dental phobia and vasovagal reflex following an atrioventricular junctional rhythm: a case report. Sci Prog 2021. [Google Scholar] [Crossref]
- S Matsuda, H Itoi, T Ryoke, H Yoshimura. How should clinicians assess acute dental pain? A review. Medicine (Baltim) 2022. [Google Scholar] [Crossref]
- JR Shaefer, SJ Lee, NK Anderson. A vibration device to control injection discomfort. Compend Contin Educ Dent 2017. [Google Scholar]
- D Ching, FM Lcy. Effect of the DentalVibe injection system on pain during local anesthesia injections in adolescent patients. Pediatr Dent 2014. [Google Scholar]
- M Elbay, ÜŞ Elbay, S Yıldırım, C Uğurluel, C Kaya, C Baydemir. Comparison of injection pain caused by the DentalVibe Injection System versus a traditional syringe for inferior alveolar nerve block anesthesia in pediatric patients. Eur J Paediatr Dent 2015. [Google Scholar]
- R Dak-Albab, MB Al-Monaqel, R Koshha, H Shakhashero, R Soudan. A comparison between the effectiveness of vibration with Dentalvibe and benzocaine gel in relieving pain associated with mandibular injection: a randomized clinical trial. Pain Intensive Care 2016. [Google Scholar]
- M Shilpapriya, M Jayanthi, VN Reddy, R Sakthivel, G Selvaraju, P Vijayakumar. Effectiveness of new vibration delivery system on pain associated with injection of local anesthesia in children. J Indian Soc Pedod Prev Dent 2015. [Google Scholar]
- LS Uman, KA Birnie, M Noel, LS Uman, JA Parker. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev 2013. [Google Scholar] [Crossref]
- HM Whelan, AR Kunselman, NJ Thomas, J Moore, RF Tamburro. The impact of a locally applied vibrating device on outpatient venipuncture in children. Clin Pediatr (Phila) 2014. [Google Scholar]
- D Ching, M Finkelman, CY Loo. Effect of the DentalVibe injection system on pain during local anesthesia injections in adolescent patients. Pediatr Dent 2014. [Google Scholar]
- MF Sfondrini, P Gandini, M Malfatto, FD Corato, F Trovati, A Scribante. Computerized casts for orthodontic purpose using powder-free intraoral scanners: accuracy, execution time, and patient feedback. BioMed Res Int 2018. [Google Scholar] [Crossref]
