Introduction
Residual ridge is a term used to describe the shape of the alveolar ridge after healing of bone and soft tissues following tooth extraction.1, 2, 3 Residual ridge resorption is a chronic, progressive, irreversible and cumulative disease.1 Resorption is the loss of tissue substance by physiologic or pathologic processes. According to GPT 9, residual ridge resorption is defined as a term used for the diminishing quantity and quality of the residual ridge after the teeth are extracted. 1 Consequences of RRR is apparent loss of sulcus width and depth, muscle attachments are displaced closer to the crest and so on.2 Stability is defined as resistance to horizontal displacement of prosthesis. Providing a stable lower denture has been challenging for dentists. 4
Here, in this article the management of the mandibular ridge resorption is described using Dynamic impression technique.
Case History
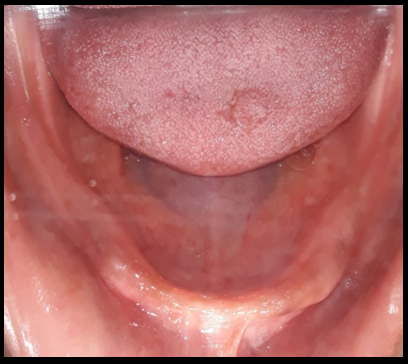
A 52 years old (Figure 1) female patient reported to the Department of Prosthodontics and Crown and Bridges, with a chief complaint of difficulty in chewing food due to loose & unstable dentures since last 1-2 months. History revealed that the patient was wearing complete dentures since 1 year and was unsatisfied with the previous denture. On examination of old denture it was revealed that both the dentures were under extended, maxillary denture in posterior palatal seal region and mandibular denture in distobuccal flange on the right side. Medical and family history was not relevant. Intraoral examination revealed Cawood and Howell Class V (low well rounded) resorbed mandibular ridge in posterior region and Atwood Order IV (knife edge) in mandibular anterior region (Figure 2). Maxillary ridge revealed Cawood and Howell Class III (well rounded) in anterior and posterior region.5
As the mandibular ridge was resorbed and patient was unsatisfied with the previous dentures, the treatment plan for the fabrication of complete denture formulated was conventional technique for maxillary ridge and dynamic impression technique for mandibular ridge.
Treatment for this patient is outlined under the heading of the various clinical and laboratory visits.
Clinical Visit 1
Primary impressions for maxillary and mandibular arch were made with impression compound.
Visit 1 (laboratory)
Beading and boxing of the primary impressions were done and primary models were poured and an acrylic maxillary custom tray 2mm short of the vestibule was fabricated for conventional border molding.
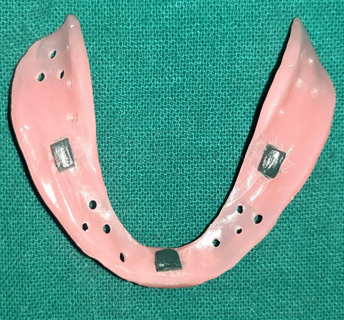
For dynamic impression, a mandibular acrylic custom tray was fabricated with one sheet of baseplate wax as a spacer and two stub handles in premolar and molar region (Figure 3). After polymerization of custom tray, spacer wax was removed followed by perforation with round bur No. 6 as the final impression material was made with alginate. Stops were made by melting thermoplastic material on the tissue surface of the tray and then pressing it carefully against preliminary cast until a space of 2 mm is achieved. The tray and cast were cooled, the tray from cast was removed and three stops were carved to required dimensions, one in the central incisor region and two in the molar region on each side (Figure 4).6
Dimensions of the stops were:6
Clinical Visit 2
Maxillary border molding was done with low fusing impression compound and final impression was made with zinc oxide eugenol paste. Mandibular final impression was made with alginate impression material in accordance to Dynamic impression technique (Figure 5). Mandibular rests were placed on the occlusal surface of the tray in the molar region. The stub handles in premolar and molar region of resin support the thermoplastic material, which was added in a columnar shape. While the thermoplastic material was still soft, the tray was placed in position on the lower ridge in the mouth and the patient was asked to close the jaws slowly. The upper residual ridge formed an impression in the soft thermoplastic material at a height corresponding to the rest position of the mandible. The tray was removed from the mouth and cooled. For Dynamic impression, alginate was manipulated with 50% excess water so as to obtain desired viscosity. Tissue to be included in impression was covered with abundant amount of material before tray was positioned in mouth and recording was done by asking the patient to close mouth till the rests had obtained firm contact with the maxilla and instructed to run the tongue along lips, suck in cheeks, pulling in lips and swallowing by keeping his mouth closed, as in closed mouth impression technique, till the impression material sets.1, 4, 6, 7
Visit 2 (Laboratory)
After beading and boxing, both maxillary and mandibular final impressions were poured with dental stone. Temporary record bases were fabricated with autopolymerizing acrylic resin and occlusal rims were fabricated on maxillary and mandibular master cast.
Clinical Visit 4
Try-in was carried out and visibility, esthetics, phonetics, occlusion was checked.
Discussion
Due to ridge resorption, the muscle attachments are located near the crest of the ridge, with greater dislocating effect of the muscles. For these reasons, the range of muscle action, and the spaces into which the denture are often extended without dislocation must be accurately recorded within the impression. These impressions can be made by utilizing dynamic methods or recording the functional position of the muscles.4, 8 The success of a complete denture relies on the principles of retention, stability and support. The prosthodontist's skill lies in applying these principles efficiently in critical situations.7
In this case report, the Dynamic impression technique was used to obtain mandibular definitive impression. Dynamic dentures differ characteristically from conventional dentures, as the borders of the denture base from a dynamic impression are longer lingually and buccally in relation to the amount of extension obtained from a conventional impression.6
Tryde et al. have suggested the three methods of impression making.6
Impression method 1: Perforated acrylic custom tray is used for the impression.
Impression method 2: An old lower denture can be used as impression tray, when opposing natural or artificial teeth are present. Perforation, stops and rest built.
Impression method 3: Denture is 1st processed on basis of conventional impression, mandibular rests are added, Correct dynamic impression is made in denture base to reshape and complete final design and then denture is relined.
In our case we have opt for impression method 1, as the patient was unsatisfied with the previous denture. In impression method 1, perforated impression tray: 6
Must not interfere with active muscle movements,
Must permit a correct thickness of impression material, and
Should stabilize the mandible in a correct position in reference to the maxillae
Stops carved on tissue surface with thermoplastic material which permit proper thickness of the final impression and proper orientation of tray on the residual ridge during impression making. Mandibular rests were made from thermoplastic material were placed over the mandibular stub handle and which helps to stabilise the tray in position by preventing anteroposterior and mediolateral displacement during definitive impression. 6, 7
Advantages of Dynamic Impressions: 6
Avoidance of the dislocating effect of muscles on improperly formed denture borders.
Complete utilization of the possibilities of active and passive tissue fixation of the denture.
Impression material being shaped by the functional movements of the muscles and muscle attachments that border the denture base are the direct results of advantages of this impression technique.
Conclusion
In resorbed cases, stability of complete mandibular dentures is major concern for both, dentists and patients. Thus, this article presents the clinical significance of using dynamic techniques for managing resorbed mandibular ridge, as this impression technique helps to record the range of action of the muscles and other structures that relate to the denture space by a functional impression using closed mouth technique. Thus, the denture are often shaped accordingly exhibiting better retentive feature, stability and overall patient’s satisfaction.