Introduction
Gingival recession is the term for the exposure of root surface by an apical shift in the position of gingiva which results in impaired esthetics and hypersensitivity.1 The goal of treating gingival recession is to cover the exposed root surface and arresting the progression of tissue loss. width of keratinized gingiva, and assessment of gingival biotype. 2 The management of gingival recession (GR) has evolved into a crucial therapeutic issue as a result of escalating esthetic and functional demands of patients. A variety of periodontal plastic surgical procedures have been developed with promising results for root coverage which Produces predictable root coverage, but healing results in formation of a long J.E with minor amounts of C.T attachment, with little or no new cementum or bone. 3, 4 Principles of Guided Tissue Regeneration was used for recession coverage along with regeneration of entire attachment apparatus. The mere use of barrier membranes have now evolved into the incorporation of correct signalling molecules like GFs & presence of correct cell population like stem cells, fibroblast & cementoblast for pdl regeneration. Recently, fetal derived MSCs from placenta or gestational tissues like amniotic fluid, umbilical cord are novel materials with rich stem cell reserves. Membranes of human placentas have been used in the field of medicine for skin grafts, treatment of burns, and ulcerated skin conditions with great success. The use of placenta allografts in dentistry is a more recent development, with the first commercial product being made available in 2008. 5, 6
The chorion is the outermost fetal membrane around the embryo in mammals, birds and reptiles. It develops from an outer fold on the surface of the yolk sac, which lies outside the zona pellucida (in mamma Fetal membranes are comprised of amniotic and chorion tissues. 7 The chorion forms the outer limits of the sac that encloses the fetus and is composed of different types of collagen and celladhesion bioactive factors. fibroblast growth factor, and transforming growth factor-b, that promote periodontal regeneration. Hence a chorion membrane is an appropriate biomaterial to be used in GTR. 8 The clinical application of chorion membrane for GTR, while fulfilling the current mechanical concept of GTR, amends it with modern concept of biological GTR. 9, 10, 11, 12, 13, 14
Case Report
A 36 year old female patient reported to the Department of Periodontics, Government dental college Trivandrum, presented with the chief complaint of receeding gum of upper left front tooth which was esthetically unacceptable to her. She also reported sensitivity for that tooth. On examination, a vertical gingival recession depth of 3 mm, clinical probing depth of 1mm and thin gingival biotype were assessed on upper left canine. (Figure 1). She was systemically healthy. Routine blood investigations and intra oral periapical radiographs were taken. IOPA revealed crestal bone loss. GRD, PD, CAL, and KTW measurements were performed at the midbuccal point of the involved teeth. A Hu-Friedy periodontal probe (UNC-15 periodontal probe) was used for all clinical measurements. In both the cases, taking into consideration the amount of vestibular depth and the presence of optimal quantity of keratinized tissue available, Chorion membrane combined with coronally advanced flap was considered as the treatment option. Written informed consent for periodontal surgery was obtained.
Case Management
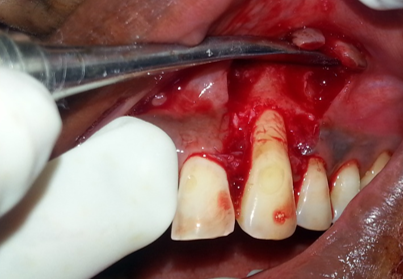
After obtaining adequate local anesthesia, two horizontal beveled incisions were made, mesial and distal to the recession defect located at a distance from the tip of the anatomic papillae equal to the depth of the recession plus 1mm. After that two beveled oblique, slightly divergent incisions, starting at the end of the two horizontal incisions and extending to the alveolar mucosa (Figure 2). The trapezoidal-shaped flap was elevated in the coronal–apical direction. For coronal advancement of the flap, a periosteal releasing incision was made. Coronal mobilization of the flap was considered adequate when the marginal portion of the flap could passively reach the level coronal to the cemento-enamel junction of the tooth. Facial soft tissue of the anatomic interdental papillae coronal to horizontal incisions was de-epithelized (Figure 3). The exposed root surfaces were thoroughly planed with Gracey curettes and was conditioned with doxycycline for 2 minutes to remove smear layer and then rinsed with normal saline. The chorion membrane trimmed to the desired dimensions was placed over the defect covering the root surface (Figure 4). Membrane was found to adhere to the root surface and no attempt was made to suture the membrane independently. Following this, the flap was repositioned 1-2 mm coronal to the CEJ, covering the tip of the de-epithelialized papillae to compensate for the expected postsurgical wound contracture and sutured with 5-0 n resorbable suture (Figure 5). A periodontal pack was placed to protect the surgical site.
Postsurgical treatment and follow-up
Postoperative instructions were given. The patient was instructed to avoid brushing and flossing in the area of surgery and to consume only soft food during the first week. Amoxicillin 500 mg TDS and Ibuprofen 400 mg TDS for 5 days were prescribed to the patient. A 0.2% chlorhexidine digluconate mouth rinse was prescribed daily for the first 15 days. Only soft food diet for the first week was advised. The sutures, were removed 10 days after surgery. The patients were instructed to resume mechanical tooth cleaning of the treated areas using a soft toothbrush and a careful roll technique after 3 weeks of surgery (Figure 6), and was recalled 2 months (Figure 7), 6 months after suture removal.
Discussion
The ultimate aim of any therapeutic approach aimed at root coverage should be to restore the tissue margin at the cementoenamel junction (CEJ) and to achieve an attachment of the tissues to the root surface so that a normal healthy gingival sulcus with no bleeding on probing and a minimal probing depth is present. 15, 16
The Connective Tissue Graft technique is considered as the gold standard in the management of recession defects. 17 However, the CTG procedure in the treatment of multiple recessions has got some demerits due to the great discomfort to the patient when large grafts are harvested from the palatal mucosa. Also, large grafts can impair vascular exchange between the covering flap and the underlying receiving bed, and thus, increase the risk for flap dehiscence and unesthetic exposure of the graft. 18
Among these methods the most commonly employed is the ‘coronally repositioned flap’ introduced by Bruiestein in 1970 and modified by Allen & Miller in 1989. The coronally advanced flap is a root coverage surgery that does not involve a palatal donor site and it has been demonstrated to be a safe and predictable approach. The CAF is the first choice when there is adequate keratinized tissue apical to the root exposure. With this approach, the soft tissue used to cover the root exposure is similar in color, texture, and thickness to that originally present at the buccal aspect of the tooth with the recession defect; thus, the esthetic result is more satisfactory. But sites treated with CAF alone has been reported with poor long term stability. So regenerative techniques are combined with CAF to improve the predictablity. GTR-based root coverage procedures have emerged as an attractive treatment because it may not only achieve similar results to those of traditional techniques, but also demonstrate histologically new attachment formation. Collagen layers of chorion are rich in collagen types I, IV,V, and VI, proteoglycans, laminin, and fibronectin. Collagen is bioabsorbable, and biocompatile, encourages migration of adjacent autogenous connective tissue, and has epithelial cells over its surface. 19, 20 Laminins exhibit a variety of biologic activities, including promotion of cell attachment, growth, and differentiation of a number of cel types. Fibronectin is involved in many cellular processes, including tissue repair, blood clotting, cell migration, and adhesion. Based on these properties, chorion membrane was used for root coverage and gingival biotype enhancement. 21 Gingival biotype was assessed because it is an important parameter when defining the qualitative nature of gingiva. In this case report, gingival thickness was augmented together with 100% root coverage, which was in harmony with the adjacent tissues. Because chorion consists of various adhesion molecules, such as laminins, thus making it even easier to use because of its superior adapation and adhesive properties. Unlike cadaveric allograft, xenograft, and alloplast barrier membranes, placental allografts have an advantage because they are composed of immunoprivileged tissue. 22
Conclusions
The results of this case report indicate a stable result at 6 months as by approximately 100% root coverage is evidenced, which could be attributed to the regenerative potential of the membrane due to the presence of mitogenic factors and anti-inflammatory proteins. The chorion membrane covered by a modified CAF is a new approach that shows excellent results in terms of root coverage, increased width of keratinized tissue & gingival biotype thickness. Chorion membrane seems to be a promising novel tissue engineered biomaterial, an effective adjunctive option for root coverage procedures. 23