Introduction
The erosive lesions of the mandible may be of odontogenic or non odontogenic origin and have different destructive capacity. The inflammatory lesions are usually associates with pain; where as destructive lesions may not show initial signs of pain. The age of patient, content of lesion, extension and expansile nature of the lesions all will contribute to diagnostic consideration factors. The progression of the lesion sometimes may be very aggressive which may rapidly change radiological appearance of the lesion.
Case Report
A 35 year old woman reported to department of Oral Medicine with complaints of pain in the right side of the face. The presentation of the pain was sharp, intermittent and spikes on stimulation which was mimicking to neuralgic type. History revealed that patient was under medication for neuralgia since two weeks. Intra oral examination revealed mild expansion of buccal cortex in lower right posterior teeth region. The extra oral examination revealed a diffuse swelling on the right angle of the mandibular region. The swelling was tender and it accentuates on palpation even on slight touch (Figure 1, Figure 2).The pattern of pain would mimic to neuralgia but the presence of the swelling was the diagnostic riddle.
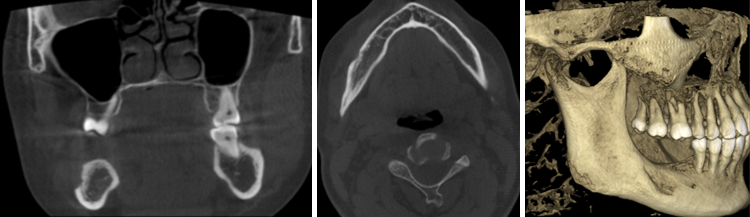
CBCT revealed destructive area on right posterior area of the mandible. The buccal cortex was lost with the hypodense area of irregular bony erosions in the molar area extending deep up to the mandibular canal (Figure 3). The radiographic features were suggestive towards a aggressive lesion and the association of the pain would suggest ourselves as an inflammation or osteolytic lesion. It was decided to surgically explore the lesion. The exploration revealed extensive presence of granulation tissue in the lesion site. The whole region was curettage and the specimen was send for biopsy.
Discussion
Lesions which occur in maxillofacial region especially maxilla and mandible is quite challenging to diagnose because of its similarity in the radiographic features.1 The lesions can have either odontogenic or non –odontogenic origin which can result in either osteoblastic or osteolytic response. These response present with various forms such as osseous demineralization, rarefaction or remodeling of bone.1 In cases with expansile, erosive and osteolytic mandibular lesions indicates the aggressive tumors such as osteomyelitis, osteosarcoma, multiple myeloma, Non Hodgkin’s lymphoma, Ameloblastoma, Langherhan cell histiocytosis and metastatic disease should be considered .Neurological involvement and cortical erosion indicates the aggressiveness of the lesion. 2 Radiographs of LCH in the jaw are challenging to interpret because the disease may mimic a wide variety of conditions, such as periapical cysts, odontogenic or non-odontogenic tumors, osteomyelitis, vascular malformations, and malignancies. 3 Pain and swelling of the affected area occur most commonly. Other findings are related to the bone involved. Clinically and imaging studies can point out malignancy or infection. Here in we report a case of Langerhans cell histiocystosis of mandible which mimicks as osteomyelitis. LCH is a rare and heterogeneous group of diseases of unknown etiology. LCH comprises the neoplastic proliferation of Langerhans cells, which are dendritic mononuclear cells usually found in the epidermis, mucosa, lymph nodes, and bone marrow.3 Studies showed male predominance (M: F=6: 11) . LCH can be found in any age group; however, children younger than 15 years of age are predominantly affected2. LCH can present as a solitary lesion or as multiple lesions within a single organ, and it can also occur in multiple organs in a single patient. LCH most commonly affects the bone, although it may also affect the skin and lymph nodes. Among the most commonly reported systemic symptoms are development of a soft tissue mass, bone pain, skin rash, fever, and lymphadenopathy. In LCH of the bone, common sites were vertebral bodies, long bones, and mandibles in children patients and the cranium and ribs in adults. Only about 10% of cases were arising from the jaw. In the present study with LCH of the jaw, all lesions were located in the mandible, particularly in the mandibular body and ramus. Previous studies also showed that the most common location in the mandible was the posterior region. Patients usually present with a toothache, tooth mobility, and symptoms associated with periodontal disease, such as swelling, bleeding, gum ulceration in alveolar LCH, floating teeth, sore mouth, jaw pain, facial swelling, delayed healing, and mental nerve paraesthesia are also reported in the literature. Literature reports, radiographically, LCH jaw lesions are divided into alveolar and intraosseous types. The radiographic features of intraosseous LCH are central osteolytic destruction with an expansion of the jaw, periosteal reaction, or fracture of the cortical bone. Because of these features, intraosseous LCH could be mistaken for many other conditions, such as an odontogenic cyst, a tumor, osteomyelitis, and even a malignant tumor. Most of the lesions showed ill-defined osteolysis with adjacent sclerotic changes on panoramic radiographs. In the present study, we analyzed CBCT images of gnathic LCH. The image shows an expansile lesion with periosteal new bone formation, bony erosions, sclerosis of adjacent bone, fluid attenuation within the lesion. Aggressive lesion presents as areas of multiple irregular bony destruction with non corticated border involving buccal and lingual cortical plates. The histopathologic features of LCH includes, a variable number of eosinophils, neutrophils, plasma cells, lymphocytes, and multinucleated giant cells are observed in LCH lesions. To distinguish LCH from other inflammatory lesions, lesional Langerhans cells need to be identified using immunohistochemical staining of CD1a or CD- 207. Considering the major symptoms of LCH are swelling and pain, the differential diagnosis of LCH from osteomyelitis might be even more difficult. The differential diagnosis for osteolytic lesions of the jaw with surrounding inflammatory changes should include LCH.
Contribution
This work was carried out in collaboration among all authors. Authors AP and PS conducted the clinical procedures of the study and prepared the manuscript. Authors RVP, VKM and LKC assisted in clinical procedures and prepared the primary draft of the manuscript. Authors PS and AP conducted the radiological investigation and gathered evidence for the treatment plan.