Introduction
Wound repair is a process that involves careful and methodical activation of basic biologic processes, key to an uneventful healing of tissues, i.e, inflammation, multiplication and proliferation of cellular structures; deposition of extracellular matrix and remodeling of tissue both biologically and functionally. Correct approximation of handling of tissues during the early stage of wound healing is detrimental for proper healing.1 The term “suture” describes any strand of material utilized to ligate blood vessels or approximate tissues. Sutures provide a temporary means of approximating defect edges to promote wound healing. Final cosmetic results depend on many variables, but suture technique is the most important one. The ideal suture technique should approximate and evert wound edges, provide prolonged support, leave no suture marks, and be easy to place.2
The primary objective of dental suturing is to position and secure surgical flaps in order to promote optimal healing (first / primary intention) provides support for tissue margin until they heal, without dead space and reduce postoperative pain.3 When used properly ,surgical sutures should hold flap edges in apposition until the wound has healed enough to withstand normal functional stresses.4 Accurate apposition of surgical flaps is significant to patient comfort, hemostasis, reduction of the wound size to be repaired and prevention of unnecessary bone destruction. During the closure portion of conventional periodontal surgical therapy, the art of suturing allows for the precise positioning of the mucoperiosteal flaps.4
However, despite the availability of a wide range of suture materials, there is no single suture material that would be suitable for all types of surgical and medical requirements. Demands for suture materials are on rise due to an increase in the number of surgical procedures performed worldwide regardless of the availability of suture substitute such as suture staples, glues and strips in the market.3
Historical Background
The technique of closing wounds by means of needle and thread is several thousand years old. The history of surgical sutures can be traced back to ancient Egypt and the literature of the classical period contains a number of descriptions of surgical techniques involving sutures. Before catgut became the standard surgical suture material towards the end of the 19th century, many different suture paths had been followed to find a suitable material for sutures and ligatures. Materials that had been tried included gold, silver and steel wire, silk, linen, hemp, flax, tree bark, animal and human hair, bow strings and gut strings from sheep and goats.3
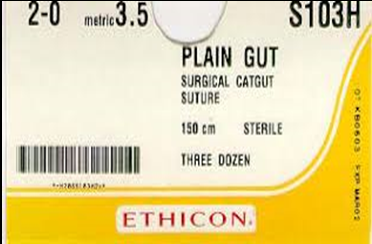
Acharya Sushruta considered as a pioneer of ancient Indian surgery has described various surgical procedures including suturing techniques. He suggested the use of horsehair, cotton and leather for wound closure. History says that some cultures witnessed the use of ants and beetles as wound closure agents. Egyptians used linen sutures along with natural adhesives to achieve proper healing. Later on sutures made of silk (Figure 1) and catgut (Figure 2) were widely employed. Hippocrates the Father of Medicine developed plant based sutures. It is also reported that he used gold wires for sutures. Joseph Lister introduced the suture material, chromic catgut in 1881.5
Requisites for suture materials
Pliable for ease of handling and knot security
Predictable performance
Prevent or limit bacterial adhesion and proliferation
Not carcinogenic
Biologically inactive
Sterilizable
Appropriate elasticity
Nonreactive
Adequate tensile strength for wound healing
Chemical biodegradability as opposed to foreign body breakdown.6
Sutures are classified as absorbable or non-absorbable, monofilament or multifilament and whether they are made from natural or synthetic material. Braided or multifilament sutures have a number of strands woven together. The non-braided sutures cause less reactivity in the body and are less prone to becoming infected because they lack grooves and rough surface for things to adhere but have the disadvantage to loosen at the surgical knot with the lack of grip.7
Principles of suturing
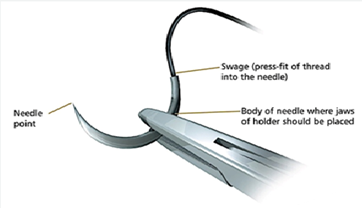
The needle holder should grasp the needle at approximately 1/3 of the distance from the end (Fig.3).
The needle should enter the tissue perpendicular to the surface. If the needle pierces the tissue obliquely, a tear may develop.
The needle should be passed through the tissue following the curve of the needle
The suture should be placed at an equal distance from the incision on both the sides and at an equal depth.
The needle should pass from the free tissue to the fixed
The distance that the needle is passed into the tissue should be greater than the distance from the tissue edge.
Avoid excessive tissue bites with small needles, as it will be difficult to retrieve them.
The tissues should not be closed under tension, since they will tear or necrosis around the suture. If tension is present the tissues should be undermined to relieve it.
The suture should be tied so that the tissue is merely approximated and the edges are everted.
The knot should not be placed over the incision line
A complication can be defined as a secondary disease or condition developing in the course of a primary disease or condition.8 The initial reaction of the tissues is a reflection of the amount of injury inflicted by passage of the needle and suture.9 Tissue reaction is reflected through an inflammatory response, which develops during the first two to seven days after suturing the tissue.10 As a result of the penetration trauma, the tissue reaction after suturing peaks at the third postoperative day. Both resorbable and non-resorbable threads result in comparable penetration trauma.11
Suture related complication is known to arise commonly from suture breakage which results in inappropriate flap approximation. If sutures are too loose it could lead to exposure of GTR membrane or graft displacement or if they are too tight then it leads to devitalisation of tissue. Also, type of suture should be chosen carefully as monofilament sutures are considered more sterile than the braided suture because of the “wicking effect” of braided sutures that pulls the bacteria & fluid into the wound site.8
Suture substitutes
Sutures are used in an attempt to improve the speed of healing and different types of materials can be used to close wound, which range from special glue to wire staples and from animal protein to synthetic materials. The choice of particular suture material should be based on the patient, the wound, the tissue characteristics, the anatomic location and evidenced based medicine.12
The goal of wound closure is to bring the edges of the wound together not only with sufficient strength to prevent dehiscence, but also with minimal residual tension and compression of the tissue to promote healing with a cosmetically acceptable scar. At the same time, there are two effects associated with suturing techniques that need to be addressed. First, the knot tying process leads to residual forces and distortion of the tissue that may impair blood perfusion through the capillaries and can compromise the healing process. The second is the body’s natural response to a foreign material which can provoke a significant inflammatory response, particularly at the knot site.12 Several suture substitutes are available today to overcome suture related complications during healing phase.
Tissue adhesives are an attractive alternative to sutures for wound closure. The surgeon applies the liquid adhesive directly over apposed defect edges. The adhesive forms an instant chemical bond with the skin to create a seal over the wound edges, thereby protecting the wound from microbial invasion and inhibiting bacterial growth. The adhesive dries rapidly and effectively glues the defect edges together until the adhesive peels off over a period of 1 to 2 weeks.2
Fibrin glue is “Fibrin Fibronectin Sealing System (FFSS)”. It is available as two component system: first component contains highly concentrated fibrinogen, factor XIII, fibronectin, and traces of other plasma proteins. The second component contains thrombin, calcium chloride, and antifibrinolytic agents such as aprotinin. Mixing of two components promotes clotting with the formation and cross-linking of fibrin.13
Surgical strips eliminate the need for transepidermal sutures over defect edges directly apposed with buried stitches. These strips can be left in place for a week or more depending on the mobility of the surgical site, the type of strip used, and whether a pre application liquid adhesive was used before strip placement.2
Disposable mechanical skin staplers are a rapid and effective method for closing long skin incisions. A three- to four-fold reduction in the time for skin closure was noticed with staple use for wound closure; however, more time is required for their removal post-operatively.14
Surgical zipper is considered as a safe alternative to conventional suture material for skin closure. The zipper is useless in high-tension or wet wounds, wounds with substantial curves of more than 20 degrees and in obese patients.14
Suture-less skin closure was first evaluated by Gillman. Surgical adhesive tapes usually contain an adhesive backing consisting of iso-octo-acrylate and n-vinylpyrolidone. Adhesive tapes are used most frequently as adjunctive wound support after staples or sutures are removed, in conjunction with buried dermal sutures, or with absorbable running subcuticular sutures in low-tension wounds.14
Laser-activated tissue repair is an alternative approach for tissue repair without sutures, staples, or polymerization. In this approach, laser light absorbed by a chromophore is converted to heat, which restructures tissue proteins to fuse with the applied sealant material by means of protein interdigitation. Laser tissue sealing has shown to reduce operation and healing times, infection, and scarring compared to conventional repair.15
Conclusion
It is well recognized that sutures have been an effective and critical part of surgeries and trauma management. Suturing is essential in surgical procedure and is governed by the basic principles of surgery like aseptic technique etc. With the sophisticated surgical procedures used daily, a clinician can obtain optimum wound closure and get esthetically good results. Sutures are used in an attempt to improve the speed of healing and different types of materials can be used to close wound, which range from special glue to wire staples and from animal protein to synthetic materials.