Introduction
The Gingival complex is considered vital in facial esthetics and smile.1 Often, the clinical practitioners perform procedures to achieve gingival esthetics along with functional problems, making them a significant aspect.2 Gingival pigmentation is a major concern for a large number of patients in dental practice. The presence of such pigmentation is considered to be the normal clinical characteristic of oral tissues in most of the human beings. Among pigments melanin, carotene, reduced hemoglobin, and oxyhemoglobin are main contributors to the normal color of oral mucosa and gingiva.3, 4 Melanin, a nonhemoglobin-derived brown pigment, is one of the most common natural and endogenous pigments contributing to the color of the gums.5 Oral melanin pigmentation is considered to be multifactorial. It is seen across all the races, age groups, and is without gender predilection.6, 7 Such melanin pigmentation of gingiva became the cause of embarrassment in smile conscious individuals, thereby increasing the demand for cosmetic therapies for the treatment of the same. Different techniques have been proposed for the treatment of gingival depigmentation that was classified into methods to remove and methods to mask gingival pigmentation.8 Scalpel surgical technique is a time- tested technique and considered as the gold standard technique.
Electrosurgery
In electrosurgical technique, heat generated by transmission of high-frequency electrical energy to the tissues leads to either cutting or coagulation of tissue.9 Bleeding control, tissue contouring and less scar tissue formation favor the use of this technique for gingival depigmentation.10 However, pain and patient discomfort during the initial healing period is more with this technique.11, 12 Furthermore, it requires more clinical expertise than the scalpel surgical method.9, 13 Prolonged or repeated application can induce heat accumulation and undesired tissue destruction.9 Contact of the electrosurgical tip with the teeth, periosteum, or alveolar bone can cause damage.13
Materials and Methods
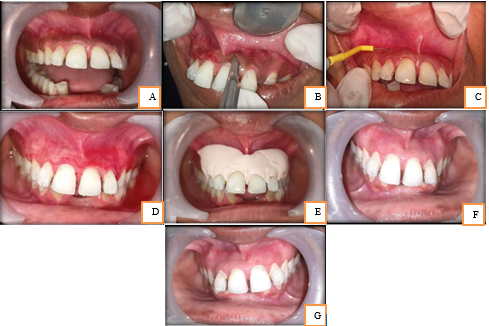
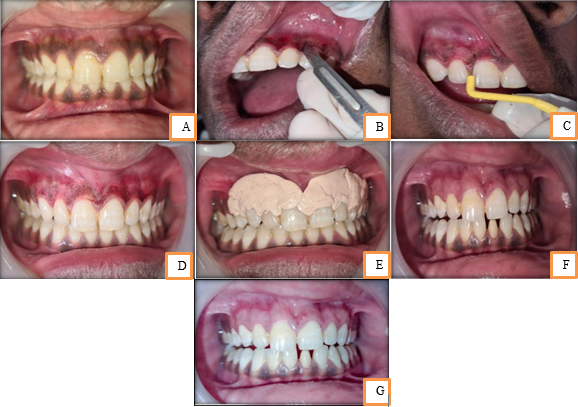
The present study is a split-mouth, randomized, comparative, clinical trial and was carried out in patients visiting the Outpatient Department of Periodontics. For patient selection, patient who were complaining about bilateral physiologic melanin hyperpigmentation of gingiva (dark gums) in the anterior segment with age ranging from 20 to 32 years were included in this study. The procedure of gingival depigmentation was planned in anterior labial gingiva of the maxilla on both sides, i.e., midline to distal of the right canine and midline to distal of the left canine. The depigmentation procedure was randomly allotted to either of the areas. The participants were informed regarding the procedure and prior informed consent was obtained. The author made sure that participants were aware of the nature of ethnic or physiologic hyperpigmentation and understood that it has no influence on the systemic health of the patient. Healthy individuals with bilateral melanin pigmentation in the anterior segment were included in this study. And were categorized as moderate or heavy clinical pigmentation as per the Dummett Oral Pigmentation Index (DOPI).14 Patients with thin gingival biotype, pregnant and lactating women, medically compromised patients, patients using drugs or chemicals that got potential to cause oral pigmentation and also patients who were under medication or condition that will interfere with bleeding or wound healing, and smokers were excluded from the study. Depigmentation procedure one week prior to the depigmentation procedure, all the enrolled participants underwent initial phase therapy, i.e., oral prophylaxis, scaling, and root planing. Since both depigmentation procedures were performed in the same patient on different quadrants, the author made sure sufficient time, i.e., the 1-week interval was kept in order to assess pain and healing patterns from two procedures. Scalpel scraping technique after achieving adequate anesthesia (using 2% lignocaine hydrochloride) on the surgical area, entire epithelium and a layer of connective tissue were scraped using surgical scalpel blade No. 15, till all the visible pigmentation were removed from margin to mucogingival junction. Bleeding from the surgical area was controlled through direct application of pressure pack and the periodontal dressing was placed [Figure 1. e and Figure 2. e ]. A radio-surgical electrosurgical unit was used for the procedure. It is based upon the bi-terminal principle which grounds the patient in the circuit. After administering Local anesthesia with 2% lignocaine hydrochloride at the surgical area, a high frequency electric current to biological tissues in order to cut, coagulate, desiccate or fulgurate tissues was applied. Its benefits include the ability to make precise cuts with limited blood loss. It involves the passage of radio-waves at the frequency of 1.5 to 4.5 mhz. The electrode was used for de-epithelizing the gingiva [Figure 1. c and Figure 2. c ]. Light brushing strokes were performed and tip was kept in motion to avoid heat build-up [Figure 2. c ]. The depigmented area was then covered with a periodontal dressing. Following the depigmentation procedure, the patient was instructed to maintain good oral hygiene and to avoid eating of any hot, spicy foods following 24 h of surgery. Moreover, they were also instructed to avoid any trauma during the healing period (4–7 days following treatment) and advised to use 0.2% chlorhexidine digluconate to rinse twice daily for 2 weeks. Patient did not report any pain or discomfort on the side treated with electrocautery after the procedure. Complete healing of wound was achieved after a week.
Clinical parameters such as bleeding, pain, wound healing, recurrence of pigmentation, and intensity of repigmentation were observed. Assessment of clinical repigmentation and intensity was done using Dummett Oral Pigmentation Index (DOPI) at 3rd and 6th months postoperatively [Figure 1. f and g, Figure 2. f and g].
Case 1
A 32-year old female patient who was concerned about her discoloured gums. Depigmentation procedure was planned accordingly for a split mouth comparison.
Discussion
A smile is determind not simply by shape, position, and color of the tooth, but also by the health of gingival tissues. 15 The manifestation of gingiva plays a crucial part and has tremendous impact on esthetics of our smile. Owing to the setback of “black gums,” there were developing esthetic concerns that require the depigmentation procedures. Scalpel surgical technique is taken into consideration as the most economic with no equipment constraints. Moreover, the healing period for surgical wounds is considered relatively faster than other technique.13, 16 Other procedure that is considered as effective, pleasant, and reliable is electrosurgery. Reduced pain and discomfort, clean and dry operating field are few advantages using electrosurgery. Therefore, the present study was designed for comparative evaluation of conventional surgical scalpel procedure and electrosurgery in terms of bleeding during procedure, pain, wound healing, and recurrence and intensity of repigmentation.
It was observed that both surgical scalpel and electrosurgery procedures provided similar results in terms of effective removal of gingival pigmentation and repigmentation when assessed at regular intervals of 3 and 6 months, respectively. When bleeding was assessed between two techniques, surgical scraping showed slight-to-moderate bleeding, while electrosurgically-treated areas exhibited minimal to none, which is consistent with previous studies.11, 9, 13
In terms of wound healing, patients had no hemorrhaging, morphological abnormalities, scarring, or infection at the surgical site. In the present study, the results from both treatment modalities were stable upto 3 months and 6 months postoperatively. Verma et al. in 2013 presented a case of gingival hyperpigmentation that was treated using a surgical blade and showed good results in terms of patient’s acceptance and in aesthetics as re-pigmentation was not noted at post-operative follow up period of 6 months.1
In another study, Shah 2012 reviewed 48 cases and treated with scalpel technique. In all the cases, the least inconvenience and most extreme patient satisfaction was achieved with complete resolutions of chief complaint and no signs of recurrence after 30 month follow up period.17 A major shortcoming of electrosurgery is that its repeated and prolonged use induces heat accumulation and undesired tissue destruction.18 Bhusari et al. 2011 evaluated efficacy of electrosurgery and scalpel technique, 3 patients were treated by split mouth design. Earliest signs of re-pigmentation started at 6 months interval and it was observed that re-pigmentation was more pronounced in electrocautery than scalpel technique.19 Prasad et al. 2005 evaluated the response of electrosurgery and combination of bur scrapping and scalpel technique. Electrosurgery showed desirable results, followed by epithelial excision and bur abrasion methods which showed a slight recurrence of pigments.20
Even though the exact mechanism for clinical repigmentation is unclear, it is believed to occur due to the migration of active melanocytes from adjacent pigmented tissues to surgically treated areas, leading to repigmentation.21 On the other hand, according to Ginwalla et al., repigmentation was attributed to left out melanocytes.22 In case series by Perlmutter and Tal, repigmentation in few cases had not occurred upto 431 days postsurgically, and in one case, it did not occur over the first 2 years. They speculated that such delay in occurrence was either due to nonmigration of melanocytes or due to inactive melanocytes that were migrated.21
Conclusion
Based on the findings, we conclude that both surgical scalpel and electrosurgery were found to be clinically effective and cost-efficient in treatment of melanin pigmentation of gingiva. Future studies must focus on melanocytic activity rather than the techniques to be used, owing to their contribution in repigmentation and also to reduce the rate of recurrence of pigmentation.