Introduction
Implant discovery has led to increase in treatment options for patients who are partially or completely edentulous. However, it has become evident that while the implant is successful in many patients, these are yet not free of post placement complications. Complications include presence of inflammation around implant including perimucositis, peri-implant bone loss, and peri-implantitis. Peri-implant was introduced in 1987, and defined as ‘a site-specific infection which shows many features which are in common with chronic periodontitis’.1 Peri-implant is classified into: peri-implant mucositis and peri-implantitis in 1992 and has been revised till present date.2
Peri-implant mucositis is considered as a state of ‘reversible inflammatory reaction of soft tissues surrounding functioning implant’, while peri-implantitis is defined as the state of ‘inflammatory reactions with loss of surrounding bone and tissues of functioning implant’.2 Peri-implantitis is a disease that severely affect an existing implant.1
Etiological factors that are most commonly associated with development of peri-implantitis which include presence of bacterial plaque and host response.3 Risk factors that are associated with peri-implantitis include smoking combined with IL-1 xenotype polymorphism, previous history of periodontitis, poor compliance with treatment and oral hygiene practices, presence of systemic diseases that affect healing, left behind cement following cementation of crowns, lack of keratinized gingiva, and any previous history of implant failure.4
Treatment of peri-implantitis include: conservative treatment approach (non-surgical) and other is surgical treatment. Peri-implantitis is classified as following -mucositis, moderate as well as severe peri-implantitis depending on severity. Treatment includes decontamination of the infected implant or previously exposed surfaces. Current evidence has shown that non- surgical therapy for peri-implantitis is minimal effective even with adjunctive use of locally or systemic delivered antibiotics.3, 4 Surgical treatment is usually required. Primary aim of surgical intervention is to allow the surgeon to instrument implant surface and perform debridement with decontamination. Decontamination and detoxification of implant surface can be performed in chemical or mechanical form.
Purpose of our case report is to present the outcome of surgical peri-implantitis treatment associated with regenerative procedures, focusing on importance of both implant surface decontamination and also reconstructive therapy with placement of xenograft so to achieve better clinical results in esthetic zone.
Case Report
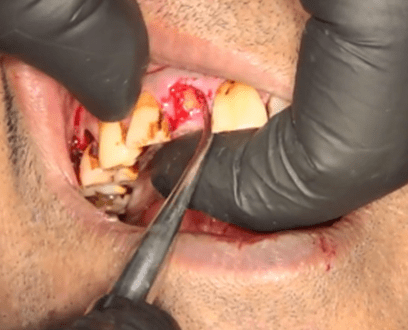
A 45-year-old male patient reported with history of trauma and crown fracture at cervical area of tooth 11 and requested for immediate solution. He was smoker, his medical history was non-significant but he had poor plaque control. Clinical and radiological evaluation showed adequate alveolar bone, and absence of periapical pathology. So, it was decided to extract the tooth and place endosseous implant immediately with placement of provisional restoration to avail the benefits like: preservation of bone and emergence profile. After administering antibiotic and analgesic, induction of local anesthesia was done using lignocaine with adrenaline. Preservation of alveolar bone is the main key in success of immediate implant. So, extraction of tooth was done. (Figure 1)
An atraumatic extraction of the tooth was done and root length was measured. The extraction socket was debrided thoroughly and evaluated for any defect or perforation with the help of a periodontal probe. [Figure 2]
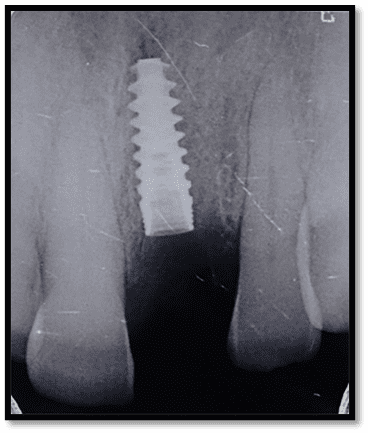
Osteotomy site was prepared with the help of sequential drills such that the implant is placed. A Noble Biocare Implant of (3.75mm × 13mm) was placed and primary stability was achieved with ISQ ranging from75-80. [Figure 3]
The patient was recalled after 4 months for prosthetic placement and was given zirconia crown over implant. Proximal contacts and occlusion was checked. The crown was then cemented using a resin modified glass ionomer cement [Figure 4]. Patient was very happy with final esthetic and functional outcome. Oral hygiene instructions were explained to patient and recall after 3 months for regular checkup.
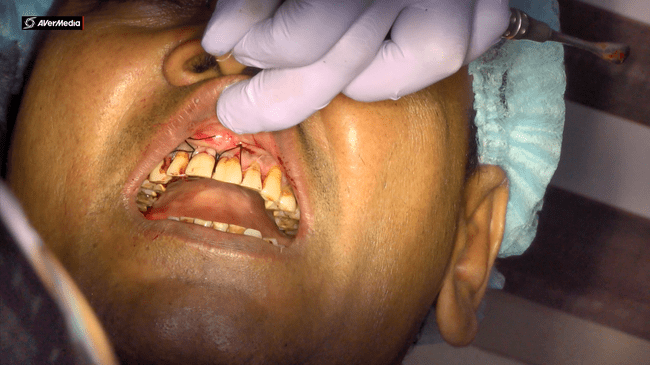
After 2 years patient reported to clinic with slight discomfort. Clinical signs included inflammation, bleeding on probing and bad smell from mouth. Upon clinical examination probing pocket depth was 6 mm around the implant with bleeding on probing. Based on clinical and radiographic findings, diagnosis was made to be as moderate peri-implantitis. [Figure 5]
The initial therapy included: non-surgical debridement with adjunctive antibiotics (amoxicillin 500 mg three times daily for 1 week) which only did minimal improvement in peri-implant soft tissue but without reductions in PD (probing depth) or BOP (bleeding on probing) and suppuration when observed upon for re-evaluation after 6 weeks. Other treatment options were discussed with the patient including continued non-surgical maintenance, regenerative surgical therapy, as well as removal of implant with site reconstruction for future implant placement. The patient wanted to retain the implant and was interested for surgical regenerative therapy. Informed consent was obtained in order to proceed with the surgical treatment.
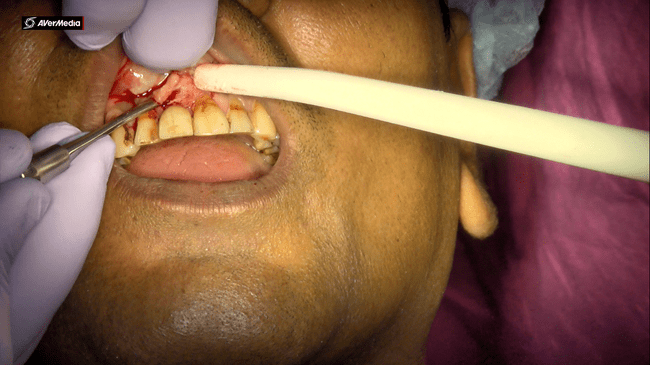
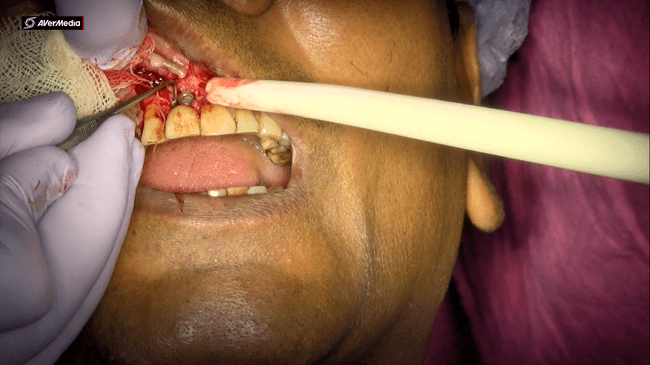
After giving local anesthesia, a full thickness mucoperiosteal flap was raised on the buccal aspect of the 11 implant [Figure 6].
Upon flap elevation, granulation tissue was observed on implant surface. Implant surface was thoroughly and carefully debrided with periodontal curettes. [Figure 7]
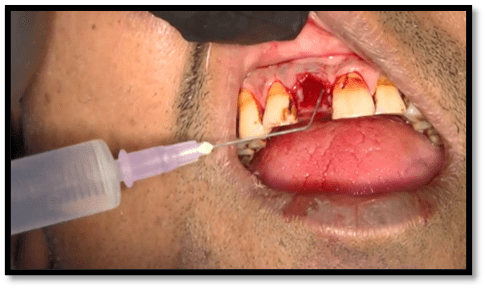
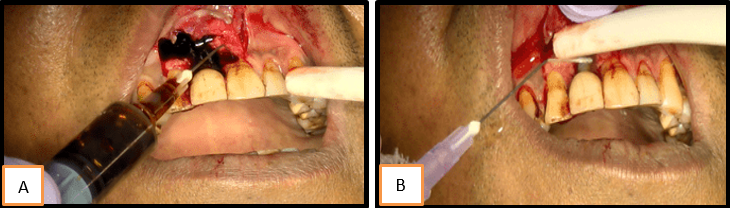
The implant crown was left in the place. Implant surface detoxification was carried out first by rinsing of the implant surface with povidine iodine followed by irrigation with normal saline [Figure 8a,b].
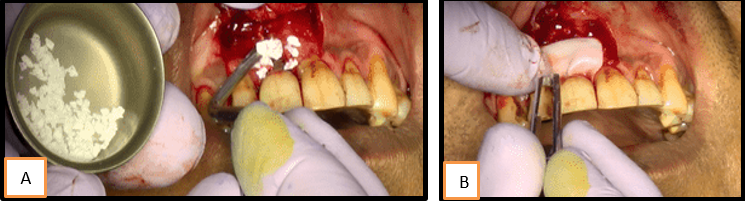
The bony defect was grafted with Geistlich Bioss (xenograft) and then covered with CREOS membrane [Figure 9a,b,c]
The CREOS membrane was adapted to the site and effectively sealing of the graft was done with surrounding tissues. Flap was closed tension-free placing a sling suture using a 5-0 monocryl suture. [Figure 10].
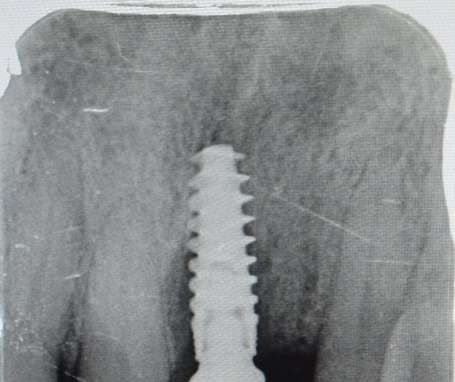
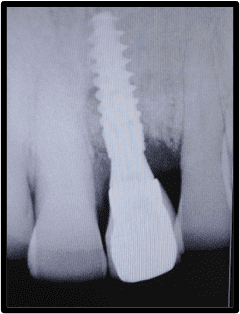
Patient was later recalled after a week for suture removal and radiograph was taken which showed graft and membrane around implant. Oral hygiene instructions were given to patient. [Figure 11]
Patient was recall after 6 months which showed uneventful healing, regeneration of bone and soft tissue as a result of placement of graft and membrane.
Discussion
Since 1970’s endosseous dental implants have become quite significant in the prosthodontics and restorative dentistry.5, 6 Despite of the many advances in techniques, materials and implant design, there is always a potential for clinical failure and hence it has been an concern both for the patient and the dentist. Dental implant failures may occur occasionally, and clinicians hesitate to perform implantation again because of the uncertain prognosis of dental implant.7 This also highlights the necessity for predictable treatment strategy for maintenance and therapy for peri-implantitis.
There is a lack of scientific guidelines for the management of peri-implantitis. As no standard protocol for treatment of periimplantitis exists, it is reasonable to present a case report using principles previously reported in studies to be efficacious for the treatment of periodontitis. 8
Main aims of peri-implant therapy are to detoxify contaminated implant surface. In peri-implant mucositis, the non-surgical methods are sufficient for detoxification which includes mechanical implant cleaning with titanium or plastic-curettes, ultrasonics/air polishing. Moreover, photo-dynamic therapy and local antiseptic medication like (chlorhexidinglukonate, hydrogen peroxide, sodium percarbonate, povidone-iodine) may support antimicrobial therapy. 9
According to the literature, it is proved that peri-implant mucositis can be successfully treated if diagnosed at initial to moderate phase. 10, 11 non-surgical therapy has not been shown to be an effective treatment of periimplantitis. 12, 13 Surgical treatment for such mucositis cases have given convincing results. However, longitudinal studies are yet to be validate treatment modality which may be optimal, given the different clinical scenario. Apart from all surgical modalities, monitoring of dental implants acts as essential part of treatment. Thus, periodontal evaluation and maintenance is necessary. Moreover, patient’s motivation for oral hygiene care and positive attitude towards treatment plan helps to overcome peri-implant complications immediately after implant placement. 14, 15
In present case decontamination process has proven to be an effective treatment option when coupled with bone regeneration by graft and membrane placement. Considering present case report, it could be assumed that by use of bioabsorbable membrane may have promoted an undisturbed graft remodeling thus permitting new bone formation due to creation of space over graft against ingrowth of soft tissue cells surrounding defect. Moreover, bio absorbable collagen membrane is used in present case may have decreased risk of membrane exposure, allowing an uneventful healing as demonstrated by recall visits and final outcome.
Conclusion
Management of periimplantitis is challenging for dental practitioners and surgeons providing implant treatment. Microbial population vary from patient to patient, and has the ability to change and develop over time which makes treatment of peri-implantitis more difficult. However, combined surgical and antimicrobial protocol described in present case, which encompasses use of open flap debridement with povidine iodine/normal saline and placement of xenograft with membrane. This is viable and recommendable treatment option in case of implant showing bone resorption as a result of peri-implantitis.