Introduction
Psychosomatic disorder
Somatic Symptom Disorder (SSD), formerly known as Psychosomatic Disorder, is characterized by somatic symptoms that are either very distressing or result in significant disruption of functioning, as well as excessive and disproportionate thoughts, feelings, and behaviors regarding those symptoms.1
According to Diagnostic and Statistical Manual of Mental Disorders (DSM-5), individuals with this disorder mostly exhibit one severe symptom, which is most commonly pain, that might be of specific or non-specific nature.1 According to the newest revisions in the DSM-5, the disorder is recognized as somatic symptoms and related disorders, which include: Somatic symptom disorder, Factitious disorder, Illness anxiety disorder, and Somatoform disorder not otherwise specified (NOS). The prevalence of SSD is estimated to be 5%-7% of the general adult population, with a higher tendency of females of reporting the disorder than males. 1
Oral psychosomatic disorder
Psychosomatic disorders are identified by disturbances of normally occurring physiological processes of the human body due to emotional or mind-related aspects. 2 Oral mucosa is highly reactive to physiological influences. 2 The oral environment is related directly to human instincts, passions, and emotions and is charged with high psychological potential. 3 Hence, disorders characterized by physiological changes that originate partially from emotional factors affecting the oral cavity are called oral psychosomatic disorders. 3
An entire sphere of psychosomatic disorders which affect the oral and para-oral present but remain unrecognizable because of the limited nature of their presenting features. 4
Brain-skin axis
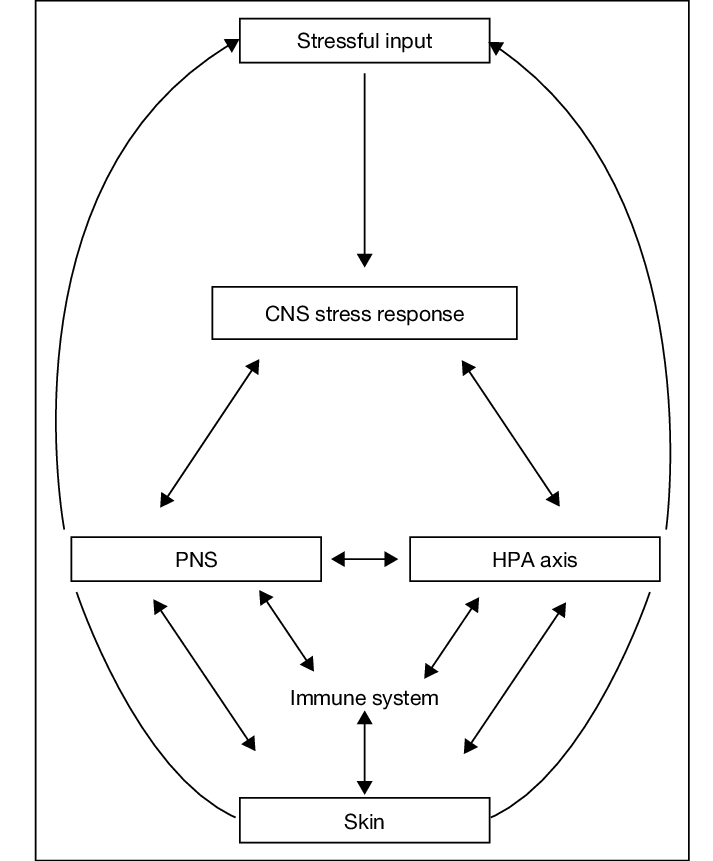
The most accepted hypothesis for the occurrence of psychosomatic disorders is the brain-skin axis concept as shown in Figure 1. Stress impairs the barrier function of the skin leading to increased inflammation and worsening of the course of various skin diseases. Psychological stressors such as financial strains, health problems, relationship conflicts at home, etc. elicit a stress response. 5 Hypothalamic pituitary adrenal (HPA) axis is the body's central stress response system that releases neuroendocrine, neurotransmitter, and neuropeptide signals upon the perception of stress. 5 Skin response by releasing inflammatory cytokines which leads to activation of mast cells. 5 This may promote neurogenic inflammation and immune regulation. 5
Classification
Classification of somatic symptom disorders with relevance to the oral cavity:
According To McCarthy and shklar6
According To bailoor and nagesh (2001) 7
Various Oral Psychosomatic Disorders
Oral lichen planus
Oral lichen planus (OLP) is a common chronic immunologic disease, inflammatory in nature, which affects the mucosa and skin. 3 This mucocutaneous disease presents itself as interlacing white keratotic lines known as Wickham’s striae, typically located bilaterally on the buccal mucosa 3 as seen in Figure 2. Women’s predilection is higher and occurs most frequently during the fifth and sixth decades of life. 4
Psychosomatic factors along with the interaction of host, lifestyle, and environmental factors play a crucial etiological role in the occurrence of different forms of mucosal changes seen in oral lichen planus.2 The cause of the disease is unknown but some authors state that it is a psychosomatic disorder caused by anxiety or stress. 2
The disease undergoes remissions and exacerbations most often relating to the patient’s emotional status. 2
Chaudhary has reported higher scores of anxiety, depression, and stress in patients with OLP in comparison to healthy controls. 4 Burkhart et al. (1997) assessed medical history, lifestyle, and health habits and pointed out the occurrence of stressful events at the onset of OLP in 51 percent of the subjects. 4
Aphthous stomatitis
Also known as canker sores, recurrent aphthous stomatitis (RAS) is one of the most common and painful diseases of the oral mucosa.8 Most common form of RAS is minor RAS which makes up approximately 80% of the reported RAS episodes. 8
The ulcers are round or oval, less than 1 cm in diameter with necrotic centers surrounded by erythematous margins8 as depicted in Figure 3. They are significantly painful and usually heal within 10-21 days. 8
Stress significantly increases the odds of having a RAS episode but does not affect the duration of the RAS episode. 8 Any history of anxiety and depression was not found to change the association between stress and RAS onset of duration. 8
Erythema multiforme
Erythema multiforme (EM) is a vesiculobullous skin lesion characterized by typical target or bull's eye lesions affecting the hands, feet, elbows, knees, etc. as seen in Figure 4. It is of 3 types - Major EM, Minor EM, and Steven Johnson Syndrome (SJS).
It often occurs in association with the herpes simplex virus.3 Deregulation of T lymphocytes occurs due to stress as a precipitating factor.3 Oral EM is characterized by the appearance of oral and lip ulcerations3 as depicted in Figure 5.
Mucous membrane pemphigoid
Mucous membrane pemphigoid (MMP) is a group of autoimmune dermatologic diseases characterized by blistering lesions which heal with scarring.10 Mucous membranes of the throat, nose, and oral cavity are most commonly affected.9
Autoantibodies are produced to attack the basement membrane of the epithelium, separating it from the underlying connective tissue, and giving rise to fluid-filled blisters.9 Stress and depression are listed as predisposing factors. 3 Oral mucosal bullae are most commonly seen as depicted in Figure 6, along with ulcerations, painful and swollen gingiva that bleeds easily, dysphagia, and hoarseness of voice. 9
Psoriasiform lesions
Psoriasis is a chronic inflammatory skin disease with systemic manifestation. 10 Its etiology is complex and multi-factorial including genetics and stress. 10
An increased stress-induced autonomic response and diminished pituitary-adrenal activity cause an imbalance of vasoactive intestinal peptides. 11 This leads to increased production of inflammatory mediators contributing to further imbalance of neurotransmitters 10 and may lead to the development of symptoms of anxiety and depression. 10
Psoriasis is characterized by patches on red, inflamed skin which are covered by silver-coloured scales affecting the skin of the extensor surfaces of arms and legs as well as the skin of the scalp. The scales are often accompanied by pruritis as seen in Figure 7.
In 44% of patients, stress has been reported as a cause of initial flare of psoriasis and up to 80% of patients have had recurrent flares due to stress.12 Depression may flare up itch perception, exacerbating pruritis.11 More severe, skin and joint symptoms have been noted in patients who report high levels of psychological stress. 11
Geographic tongue
Geographic tongue is a chronic inflammatory lesion of the tongue of unknown etiology. 12 It is also known as benign migratory glossitis or wandering rash of the tongue. 12 Geographic tongue is found to be an oral manifestation associated with psoriasis. 12 Etiological factors include allergy, bacterial and fungal infections, dietary deficiencies of iron and vitamin B as well as psychosomatic factors such as stress. 12
Lesion mainly affects the back and sides of the tongue. 12 It is characterized by white serpiginous lines around red, depapillated mucosa of the tongue 12 as depicted by Figure 8. While it is mostly asymptomatic, some patients may report pain accompanied by a burning sensation. 12
Reiter’s syndrome
Reactive arthritis, previously called Reiter's syndrome, is an inflammatory arthritis as seen in Figure 9. It occurs due to genitourinary or gastrointestinal infection. 13 It is seen to occur in association with psoriasis. 13 Joints of the ankles and knees are most commonly affected. 13 It presents as a triad of arthritis, urethritis, and conjunctivitis. 13 Tendonitis, mucosal ulcers, erythematous dermatitis and nail dystrophy are also seen. 13
Chronic periodontal diseases
The etiology of inflammatory periodontal disease is complex and multi-factorial. 14 A psychosomatic disorder exerts an influence on periodontium in two ways:
Self-inflicted injuries witnessed in these patients
Disruption of autonomic nervous system altering tissue response. 14
Mental stress has been implicated as a factor that can influence the state of periodontal health. 4 Physiologic mechanisms such as alteration in saliva, changes in gingival blood circulation, endocrine imbalances, and altered host resistance may affect and alter periodontal tissues. 4 Psychoneuroimmunologic effects were confirmed by findings of poorer immune functions in people who experienced stressful life events or chronic stress. 4 Figure 10 shows chronic periodontitis.
Recurrent herpes labialis
Recurrent herpes labials is a mucocutaneous infection caused by HSV-1. 4 It causes pain and blistering on the lips (as seen inFigure 11) and the perioral areas which are termed cold sores. 4 Stress is a precipitating factor for its occurrence. 4 In patients with recurrent herpes labialis, CD4 helper/inducer T lymphocyte count was found to be significantly lower. 15
Burning mouth syndrome
Burning Mouth Syndrome (BMS) is characterized as a painful, complex condition, which involves a burning or tingling feeling in the mouth that may occur every day for months or longer. 16 This may be accompanied by pain. 16 BMS is most commonly seen in adults over the age of 60. 16 It is thought to be about five times more prevalent in women than in men. 16
It is a multi-factorial disease where neurogenic, local, systemic, and psychogenic factors play a role.14 The wide psychogenic factors highlighted in the etiology of BMS are anxiety, depression, compulsive disorders, psychosocial stress, and cancerophobia. 14 The psychological aspects of BMS can be divided into chronic somatoform dysfunction, chronic vegetative disorders, and chronic pain phenomenon. 14
Glossodynia and Glossopyrosis
Glossodynia presents as chronic pain and glossopyrosis presents as a burning sensation, both of which commonly affect the tip and sides of the tongue. 17 It occurs in association with burning mouth syndrome, diabetes mellitus candidal infections, and hormonal changes associated with menopause. 17 Anxiety and depression rates are higher in patients who have glossodynia. 17
Xerostomia
Xerostomia is defined as dry mouth occurring due to diminished or absent salivary flow 16 as seen in Figure 12. Sreebny has defined xerostomia as a “subjective feeling of oral dryness”. 16 Xerostomia is commonly seen among older adults and has more prevalence in postmenopausal women than men. 16 Etiology of multi-factorial and the sensation of dry mouth may be considered as a subjectively felt somatic symptom. 16
Mason and Glen (1967) have stated that salivary secretion is regulated by ANS and is subjected to reflex stimulation from physical and psychic causes.4 Accordingly, xerostomia may result from 4 basic etiological factors which are: 4
Emotions, fear, excitement, stress.
Depression.
Organic diseases e g brain tumor, Parkinson’s disease.
Drugs.
Reports state that salivary cortisol is associated with depression and anxiety, and hence, salivary cortisol can be used as an essential non-invasive biological indicator of stress. 4
Myofacial pain dysfunction syndrome
Myofacial pain dysfunction syndrome (MPDS) has become a concern for both dental and psychological fields over the past two decades.4 MPDS is characterized by regional pain originating from hyper-irritable spots, which are located within taut bands of skeletal muscle, known as myofacial trigger points. 4 Broadly defined MPDS as “defective functioning of the masticatory and other associated muscles characterized by pain”. 4
Its etiology is multi-factorial and psychological factors are considered the major causative factor. 1
Schwartz was the first to suggest the psychological make-up of the patient as a predisposing factor. 4 He stated that stress was the essential cause for clenching and grinding habits, resulting in spasm of the muscles of mastication. 4 Occlusal abnormalities play a secondary role. 4
Laskin’s Psycho-physiologic theory states that MPDS occurs primarily as a result of emotional factors rather than occlusal and mechanical factors. 4
"Biopsychosocial Model" highlights the role of biological and psychosocial factors in the causation of myofacial pain.4 Moody et al, in an experimental study of 52 MPD syndrome patients and an equal number of the control group, concluded that approximately half of the cases of MPDS showed clinical signs of greater stress than the control group. 4
Atypical facial pain and odontalgia
Atypical facial pain
Atypical facial pain is a condition wherein the facial pain experienced:
Fails to respond to multiple medical and surgical interventions;
Has an incessant and severe quality that shows little variation in intensity during waking hours but does not interfere with sleep.
Pain is defined vaguely, not conforming to known anatomical pathways (such as in the case of Tic Doulourex) and not commensurate to the degree of pathological physical findings. 18 The disorder has been hypothesized by Engel to be caused by the ‘conversion’ of psychological distress into physical symptoms. 19
Atypical Odontalgia
It is a condition characterized by a toothache that cannot be explained medically.20 Symptoms include pain with no pathological changes and/or pain which is described to be much more severe in intensity in correlation to the clinical evidence found. 20 It is often found in strong association with psychological conditions such as depression, somatoform disorders, anxiety, hypochondriasis, etc. 20
Halitosis
Oral malodour or bad breath is a common concern for millions of people. 3 Some patients complain of oral malodour that is imperceptible to others and are considered to have halitophobia (delusional or psychosomatic halitosis). 3 Delusional halitosis is a psychosomatic condition in which individuals tend to believe that they have an offensive mouth odour that any clinician cannot perceive. 3
A related disorder, olfactory reference syndrome (ORS), which is called “jikoshu-kyofu” in Japan, is a condition in which a person mistakenly believes he or she exudes an unpleasant odor. 21 Phillips KA reported that 75 % of his ORS patients were preoccupied with “bad breath”. 21
Halitophobia differs from other oral psychosomatic disorders in two major respects. 21 The first is that the main aspect of the patient’s suffering is “taijin-kyofu” (anthrophobia) rather than abnormal oral sensations.21 Second, most halitophobic patients are adolescents. 21
Dysgeusia
Dysgeusia is defined as a qualitative gustatory disorder that is characterized by a distortion of taste perception. 22 Severe taste impairment ebbs the quality of life of the patient by leading to a lack of enjoyment in eating, aversion to food, and malnutrition, along with loss of muscle mass. 23 The condition is known to be precipitated by psychiatric conditions as well as depression and anxiety, 22 as corroborated by Heath et al. 24 Implications of this disorder include excessive salt and sugar intake which might be fatal for patients with chronic or metabolic diseases like diabetes mellitus, hypothyroidism. 23
Biting of oral mucosa (Self-Mutilation)
Self-mutilation as a result of persistent cheek, tongue, or lip biting (depicted in Figure 13) is often seen in the form a fixed neurosis. 25 They are commonly observed in people who are experiencing stress and require ruling out a psychogenic background. 3
Eating disorders
Eating disorders such as anorexia nervosa and bulimia nervosa are psychosomatic disorders characterized by abnormal eating patterns. 26 Primary factors in the etiopathogenesis of eating disorders are low self-esteem and generalized displeasure with bodily looks which stem from a network of psychological factors, personality traits, peer and parental pressure, and cultural differences. 26 Clinically, dental caries, pathological tooth loss, dental erosion due to chronic self-induced vomiting (depicted in Figure 14), xerostomia, palatal erythema and ulcers, and gingival and periodontal diseases are seen. 26
Cancerophobia
It is a condition where the patient has a persistent fear that they are suffering from oral cancer. It has been seen in association with depression.3
Diagnosis of Oral Psychosomatic Disorders
Anxiety disorders are a known culprit in the development of somatic symptom diseases. The prognosis of somatic diseases is linked to anxiety disorders. 27 Health anxiety (hypochondriasis) and somatic symptom disease have shown moderate and positive correlation as in a study done by Lee et al in 2014. 28 Thus, diagnosing the anxiety levels of the patients would help in the alleviation of the somatic symptom.
The various methods to determine the presence of anxiety disorders include brain imaging and various biomarkers such as cortisol levels. In non-invasive fMRI, people with anxiety exhibit higher activation in the bilateral superior temporal gyrus. 29 Giardino et al corroborated that people with various anxiety disorders exhibited abnormal activity in the frontal and limbic-paralimbic cortical areas.30 Endocrinologically, up-or down-regulation of the hypothalamic-pituitary-adrenal (HPA) axis is also seen. 31
During periods of acute stress, there is decreased salivary flow leading to a sensation of dry mouth. 32 Hence, salivary biomarkers are used for the estimation of chronic psychosocial stresses as they are reliable and non-invasive. 33 Cortisol is one of the most commonly known bio-marker used for this purpose. 33 Mean value of salivary cortisol levels in normal patients was found to be 20.39 +/- 7.74 nmol/l. 34 In patients with psychosomatic disorders, salivary cortisol levels increase by 157-230% of the initial values depending on the kind of stress. 35 Another method to determine the anxiety levels of the patient can be through various self-administered questionnaires such as the State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), Hospital Anxiety and Depression Scale-Anxiety (HADS-A), etc. 36
Treatment of Oral Psychosomatic Disorders
Oral Psychosomatic disorders refer to a state where any disease acting in the oral cavity is either caused or worsened by mental stress and other related factors. 37 Since the etiology of these disorders is correlated with mind and body, the treatment protocol involves alleviative measures from both medical and psychological fields.37 Before the appropriate medical treatment for any oral psychosomatic disorder is initiated, the patient is first examined and screened for the presence of stress and other related factors.37 Every individual experiences different medical illnesses and oral disorders due to wearing levels of mental stress. 37 These conditions can be treated and managed either through medication or surgeries, however, complete relief and cure can be only attained by removal of psychological factors like stress, anxiety, depression, and other related factors.37 Following therapies are known to be employed as an adjunct to drug therapy for the treatment of psychosomatic disorders:
Psychotherapy
This explains a voluntary relationship between the one seeking the treatment and the one who treats. 37 These aim at changing maladaptive behaviours and decreasing a sense of personal distress. 37 The patient and doctors have an interaction about the mental status and lifestyle events to help the patient get relieved from the psychosomatic factors. This is also called talking treatment. 37
Psychoanalysis
Very commonly employed to treat depression and anxiety disorder. 37 This therapy involves multiple sessions, two to six per week lasting for several years. 37 Most importantly, the doctors keep a note of all the childhood insecurities and trauma of the patient. 37
Cognitive behaviour therapy
CBT is a psychological intervention that has been used for the treatment of various oral psychosomatic disorders in dental settings. 38 The basic underlying principle of CBT is changing cognitions and behaviours that contribute to physical or emotional problems. 38 Following techniques can be employed under CBT:
Biofeedback: Treatment measure which aims to enhance the physiological functioning of the patient. 38 The patient learns to practice keeping their muscle relaxed through constant monitoring of their muscle activity. 38
Relaxation: This method aims to correct various stressful symptoms that the body is facing by employing techniques like muscle relaxation, breathing. 38
Exposure: This technique allows the patient to face fearful situations or any stimulus related to dental settings.38
Cognitive Restructuring: This method helps to realign and re-modify any distress that the patient suffers to relieve emotional problems. 38
Electroconvulsive therapy
This is employed in cases of severe anxiety, depression, and other mental conditions. 37 This technique is given for 1 month and used along with medication.37
Hypnotherapy
This is a quite commonly and effectively used method where the hypnotist understands the state of mind of the patient. 37 It helps the patient get rid of stress-related disorders like insomnia.37
Abreaction therapy
It helps to relieve emotions associated with traumatic events leading to severe stages of oral psychosomatic disorders. 37
Yoga
Stress, the main causative factor of oral psychosomatic disorder, is mainly relieved by yoga and meditation. 37 Breathing methods called pranayama comfort the muscles that are strained by stress. 37
Lifestyle Modification
Good interpersonal relationships, eating a healthy and balanced diet, exercise, and positive thinking drastically reduce the incidence of oral psychosomatic disorders. 37