Introduction
The knowledge of surgical procedure for removal of impacted mandibular third molar is one of the very firsts to be acquired by Oral and Maxillofacial surgeon. Simultaneously, this is the most common surgical procedure performed in a dental office by Oral and Maxillofacial surgeon worldwide.1 Despite being a relatively straight forward procedure, the surgical removal of an impacted mandibular third molar is often associated with a specific set of post-operative complications, which often becomes a nagging concern for the surgeon. Therefore, the incidence of specific complications should be thoroughly understood and, wherever possible, a preventive or management strategy should be applied.
Complications, such as pain, dry socket, swelling, paresthesia of the lingual or inferior alveolar nerve, bleeding, and infection are most common. 2 Proper antimicrobial treatment and oral wound care can accelerate the epithelial healing process, thereby preventing infection and chronicity of the wound. Systemic proteolytic enzyme therapy with chymotrypsin, serratiopeptidase, aprotinin, and bromelain are being increasingly used for wound healing and anti-inflammatory effects after impacted third molar surgery.
Bromelain is a blend of enzymes extracted from the stem and fruit of pineapple (Ananas comosus), and is known for its proteolytic action, which also contain components such as acid phosphatase, peroxidase, many protease inhibitors, and organically bound calcium.3 It is prepared by centrifugation, ultrafiltration, and lyophilisation of pine-apple juice. Bromelain alters pain mediators such as bradykinin, inhibiting the synthesis of pro-inflammatory prostaglandins, mainly PGE2. Its fibrinolytic action aids in the reabsorption of oedema into the blood circulation.4, 5, 6 Overall it was found to be reducing pain, swelling, and healing time. Bromelain has very low toxicity; its IgE-mediated allergenic potential cannot be underestimated. It is recommended to administer bromelain before food and daily dosage should be 750-1000mg/day in divided doses. 7 However, there is not much literature comparing bromelain with other enzymatic preparations in treatment of inflammation associated with surgical removal of the third molar.
The purpose of this study was to comparatively assess the efficacy of bromelain with trypsin-chymotrypsin in management of post-operative trismus, pain and swelling after surgical removal of impacted lower third molar.
Materials and Methods
A comparative study was performed on 50 subjects of age group 18 - 45 years, requiring surgical extraction of bilaterally symmetrical impacted mandibular third molar teeth reporting to department of oral and maxillofacial surgery of V.S Dental College and Hospital, Bangalore, Karnataka, India. Patients with systemic diseases in whom tooth extraction is contraindicated, patients who are mentally challenged and who are unable to communicate, pregnant and lactating women, patients allergic to bromelain and immuno-compromised patients were excluded from the study.
Surgical removal of impacted mandibular third molars was performed under local anesthesia (2% lignocaine with 1:80000 adrenaline) in bilaterally symmetrical impacted mandibular third molar cases. Only one tooth was removed at a time. The second tooth removal was scheduled with a minimum gap of 3 weeks to allow resolution of post-operative symptoms following the first extraction. Post operatively, all patients received antibiotics and analgesics. Bromelain 200mg was administered BD (half an hour before meal) for 5 days after the procedure on one side, while trypsin-chymotrypsin (100000) Armour units of enzymatic activity in enteric coated tablets) was administered BD (half an hour before meal) for 5 days after the procedure on the other side.
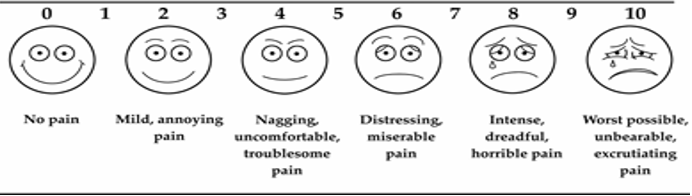
Patients were recalled on day 1, day 3 and day 7 for assessment of post-operative trismus, pain and swelling. Trismus was assessed by measuring inter-incisal distance by measuring the maximal opening between the maxillary ESUL and mandibular incisor. Pain was recorded using non caliberated 100mm visual analogue scale. The end points of the scale were ‘no pain’ and ‘pain could not be worse’. Swelling was assessed by measuring the distance between two facial reference points i.e. from tragus to the corner of the mouth.
Results
50 patients were included in our study, out of which 27 were males and 23 were females. All patients had bilaterally symmetrical impacted mandibular 3rd molar teeth. The mean age was 30.16. Each patient was given bromelain on one side and trypsinchymotrypsin on the other side. Data was analysed using SPSS software using chi square test, correlation methods to find the positivity or negativity performance of the drug. The range of the correlation lies between -1 to +1. The test used to find the significance is " t test: Two samples assuming unequal variances".
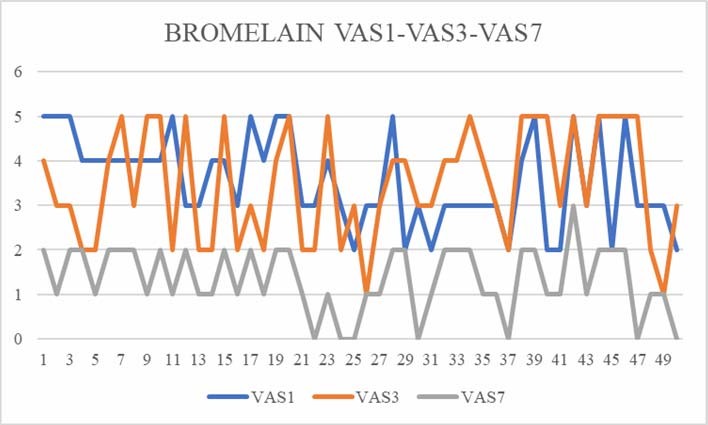
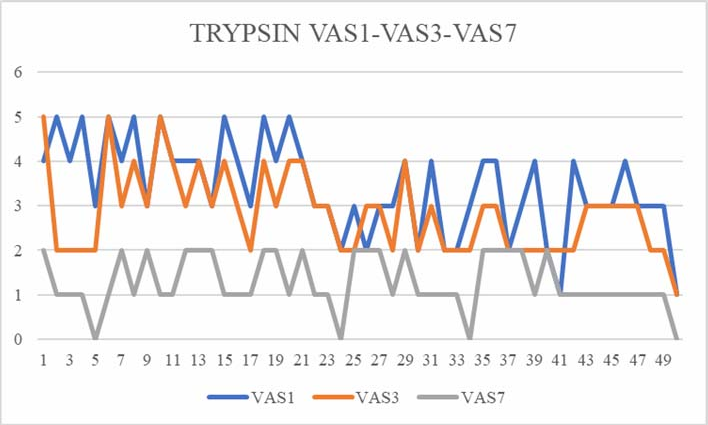
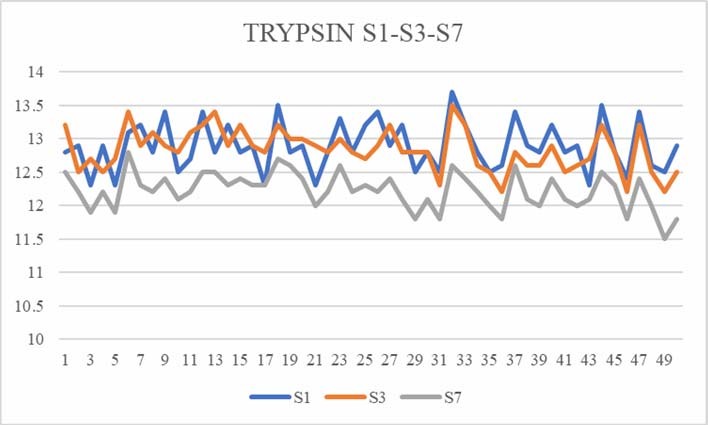
In the assessment of pain, the results showed that trypsin-chymotrypsin(0.631) showed better response in pain relief from day 1-3 compared to bromelain (0.239). However from day1-7 bromelain (0.542) was superior in pain relief compared to trypsin- chymotrypsin (0.163). [Figure 3, Figure 4].
Table 1
Table showing pain assessment scores inbromelain group
Table 2
Showing pain assessment scores in trypsin-chymotrypsin group.
Assessment of pain revealed trypsin-chymotrypsin (P-value=0.9) to be slightly better than bromelain (P-value=0.8). [Table 1, Table 2]
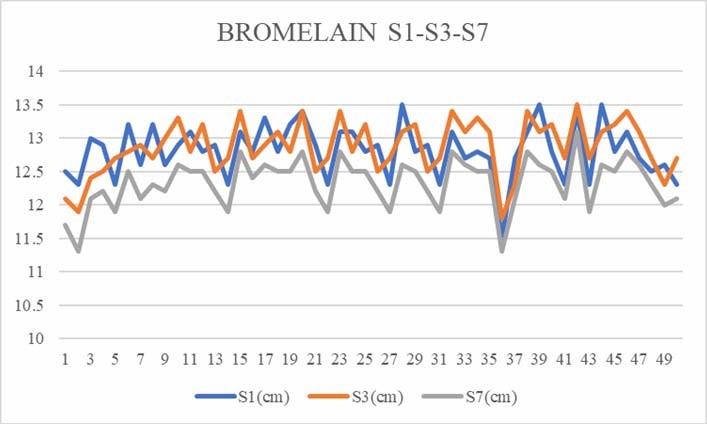
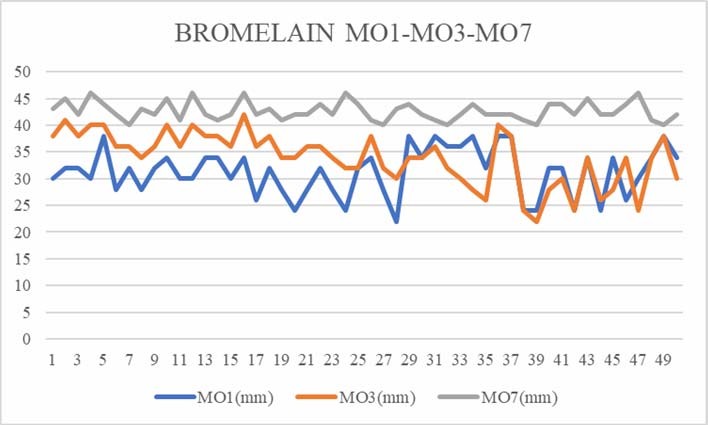
Assessment of swelling in the two groups showed almost similar response in both groups from day1-3(trypsin-chymotrypsin: 0.533, bromelain: 0.566). However from day 1-7 bromelain (0.806) was superior in reduction in size of swelling compared to trypsin-chymotrypsin (0.677). [Figure 5, Figure 6]
Table 3
Table showing assessment of swelling in bromelain group
Table 4
Table showing assessment of swelling in trypsin-chymotrypsin group
Evaluation of swelling showed similar response in both drug groups (P-value=1). [Table 3, Table 4]
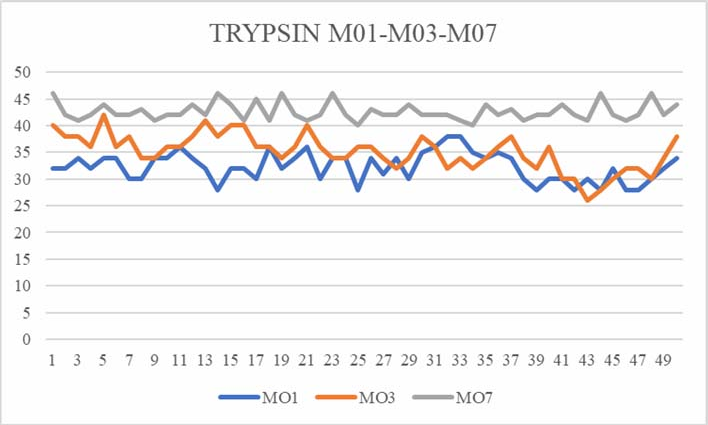
Assessment of mouth opening from day 1-3 showed better response to bromelain(0.400) compared to trypsin-chymotrypsin(0.312). From day 1-7 also bromelain(0.002) showed better efficacy compared to trypsin-chymotrypsin(-0.520). [Figure 7, Figure 8]
Table 5
Table showing assessment of mouth opening inbromelain group
Table 6
Table showing assessment of mouth opening in trypsin-chymotrypsin group
Assessment of mouth opening was found to be similar in both drug groups (P-value=0.0003). [Table 5, Table 6].
Discussion
The prevalence of third molar impaction in Indian population ranges from 18% to 32% with a slight sex predilection towards males.8 For the oral and maxillofacial surgeon, It is of utmost importance to be familiar with all the possible peri-operative complications associated with the procedure for surgical removal of impacted third molars. Impacted teeth are often associated with pericoronitis, periodontitis, cystic lesions, neoplasm, root resorption and can cause detrimental effects on adjacent tooth. The procedure of surgical removal of impacted third molars commonly involves elevating the mucoperiosteal layer, adequate guttering of the bone, and performing an odontectomy. Surgical removal of the third molar can cause severe soft tissue and bone damage and inevitably leading to the release of various inflammatory mediators like bradykinin, histamine, and serotonin, which can cause pain, swelling, and trismus.
Systemic proteolytic enzyme therapy is being increasingly used for wound healing and anti-inflammatory effects after impacted third molar surgery. These enzymes include Chymotrypsin and Trypsin (pancreatic proteases), Bromelain (pineapple enzyme), Papain (papaya enzyme), Fungal proteases and Serratia peptidase (the ‘silk worm’ enzyme). Proteolytic enzymes are administered to hasten the healing of damaged tissue and thus promote a complication free recovery. These effects are brought about by the anti-inflammatory, anti-thrombotic and fibrinolytic properties which were demonstrated both in-vitro and in-vivo. Bromelain is a proteolytic enzyme extracted from the stem and fruit of the pineapple plant. It is considerably absorbable when taken by oral route without losing its proteolytic activity and without producing any major side effects. It inhibits the synthesis of the “proinflammatory” prostaglandins without affecting that of the “antiinflammatory” properties. 9
Previously done studies have shown the effect of orally administered bromelain in reducing the postsurgical complications; these studies suggested few mechanisms of actions such as - (1) Altering pain mediators such as bradykinin, (2) Inhibiting the synthesis of pro-inflammatory prostaglandins, mainly PGE2 and (3) Its fibrinolytic action aids in the reabsorption of edema into the blood circulation. 4
Tejpal singh et.at. studied the effect of bromelain in post-operative pain after third molar extraction in a prospective randomized trial which included 40 patients. They have found that bromelain was effective 70% of the patients in reduction of pain and swelling after surgical removal of the third molar. 10
Viganò et.al., evaluated the efficacy of anti-inflammatory and analgesic properties of bromelain in oral and implant surgery. They conducted a prospective and controlled study where 300 oral surgery patients were selected, 150 of whom treated with bromelain and 150 with paracetamol and codeine. All patients who underwent placement of implants, extraction of partially or totally impacted molars, lateral maxillary sinus lift and enucleation of odontogenic cysts were included in the study. They found that in the bromelain group, inflammation, edema and trismus were statistically better than in the group that only received analgesics. 11
In our study, we noted that Bromelain when compared to Trypsin- Chymotrypsin after third molar surgery in bilaterally symmetrically impacted teeth showed considerable reduction of swelling, pain and increase in mouth opening, when compared swelling from tragus to corner of the mouth, mouth opening measured with a Vernier calliper from upper incisor to lower incisor and pain on Visual analogue scale with bromelain than trypsin-chymotrypsin.
Conclusion
In our study we can conclude that bromelain has a significant effect on swelling, mouth opening and pain after surgical removal of impacted third molar than chymotrypsin. We suggest its usage in reduction of swelling and pain post operatively in surgical removal of third molar. However further studies with larger sample size and randomizations are required to confirm the same.