Introduction
Head and neck cancer in Asia, especially India accounts for 57.5% in terms of incidence, globally. Furthermore 60-80% of patients seek medical care with a progressed condition in comparison to 40% in developed countries.1 Due to diagnosis made at advancing or severely progressed conditions, outcome and prognosis of patient is hampered with a toilsome financial burden. Verrucous Hyperplasia (VH) is a rare and potentially malignant lesion having a tendency to transform into its malignant equivalent, Verrucous Carcinoma (VC), which is clinically identical, yet histologically vacillate. 2 VC was first described by Lauren V Ackermann in 1948 though until mid-1980s it’s pathogenesis was not explored solely, 3 it was known as “Verrucous Carcinoma of Ackermann” or “Ackermann's tumor”.4 Verrucous carcinoma is better described as a well differentiated, low grade variant of oral squamous cell carcinoma(OSCC) contributes up to 2-12% of all oral carcinomas showing survival rate of approximately 50% in 5years.5 Adept cooperation and understanding between the surgeon and pathologist is a must for better prognostic outcome,6 this report elucidates an 80 year old female patient and a 42 year old male patient with a verruco-papillary growth in left and right buccal mucosa.
Case Report
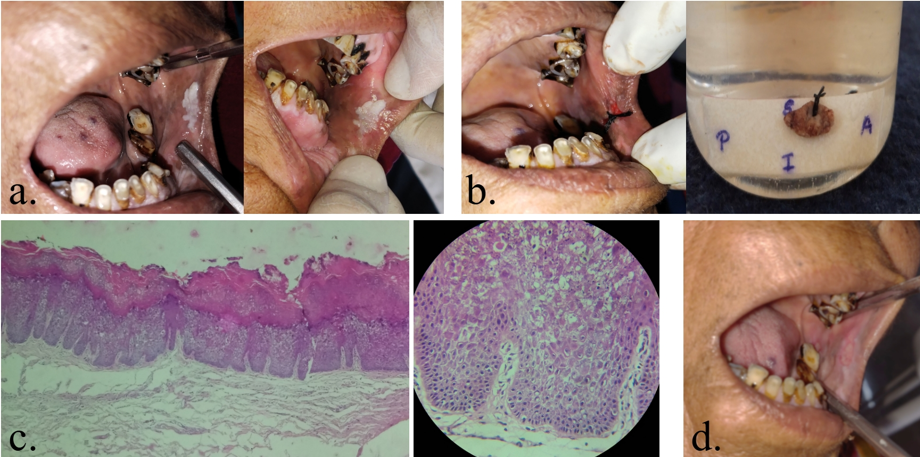
Case 1
An 80 year old female patient reported to the outpatient department of our institute complaining of a white patch in the left corner of the mouth since 3-5 months. It was gradual in onset and patient did not exactly realize when it grew. Patient was completely asymptomatic in relation to the growth. Patient revealed a tobacco chewing habit with areca nut approx 2-3 times per day since 25 years. No regional lymph nodes were palpable. Intraorally, it was a solitary well defined whitish papillary lesion, irregular in shape and measuring around 0.5X1cm in size and overlying surface showing micro-nodular corrugated texture (Figure 1a). Palpation revealed no abnormalities. Clinical diagnosis of VC was given keeping a differential of Proliferative Verrucous Leukoplakia (PVL) and VH. After hematologic and serologic investigation, complete excision was done under local anesthesia (Figure 1b). Histopathology revealed, hyperplastic stratified squamous keratinized epithelium overlying fibro-cellular connective tissue. Epithelium shows verrucous proliferation showing hyperkeratosis on the surface with prominent granular layer, broad and elongated rete ridges and dyplastic features like basilar hyperplasia, hyperchromatism was also noted (Figure 1c) giving out the impression as VH of Left buccal mucosa. Patient was advised multi-vitamins, multi-minerals and a rich diet with antioxidants and was followed up for a year. (Figure 1d)
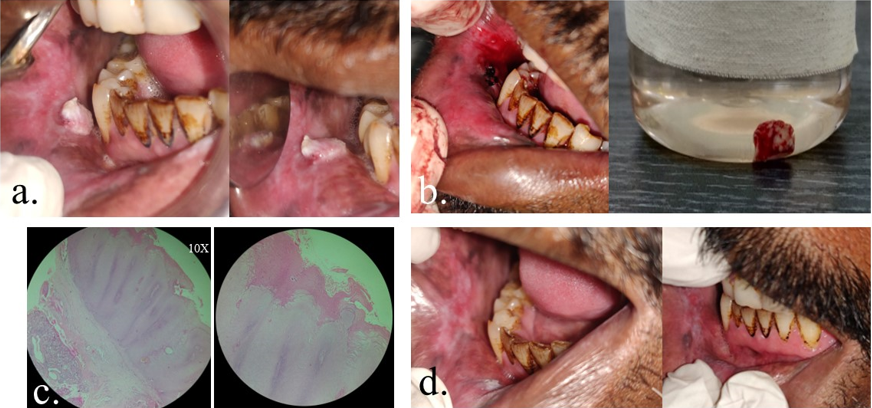
Case 2
A 42year old male patient reported to the department of oral medicine & radiology bearing a chief complaint of a growth in the right corner of the mouth since 8-10days. The onset was quite rapid and insidious and patient gave history of increasing size. No associated symptoms like pain, bleeding, but gave history of burning sensation on having hot and spicy food. Patient revealed a long standing tobacco chewing habit of having 4-5 packs per day for past 15 years. No regional lymphadenopathy was noted. Intraorally, solitary, well defined, whitish, warty in shape, papillary like exophytic growth approximately measuring 1cmx1.5cm, seen in the right commissure of the mouth corresponding to 44, 45 region. the growth is located 2cms interiorly to the commissure and 1cm below the line of occlusion & appears to be sessile, overlying surface shows roughened, small, multiple papillary like projections. Surrounding mucosa appears to be pale & stiff, mucosal changes admixed with areas of melanin pigmentation (Figure 2a), Palpation revealed no abnormalities. Clinical diagnosis of VH and Oral submucous fibrosis was put forward with a differential of VC. After running all necessary blood and serological investigations complete excision was done under local anesthesia (Figure 2b) Histopathologic examination revealed stratified squamous epithelium with verrucous surface proliferation overlying the fibrous connective tissue. Epithelium shows broad and pushing rete ridges with hyperkeratotic surface and keratin filled crypts in between & showing bland cellular features. The underlying connective tissue shows compressed dense collagen fibers (Figure 2c) giving out the final diagnosis as VC of right buccal mucosa. Patient was advised antioxidant therapy and is regularly followed up for two years. (Figure 2d)
Discussion
Intraorally, VH presents itself as a pale pinkish or partly whitish exophytic growth which possesses a warty or papillary surface which may or may not show presence of superficial ulcerations, the mean age range of incidence being 30-60 years. 7, 8 Different stages have been noted when examined histologically, which are normal mucosa, hyperkeratosis, VH, VC, papillary squamous cell carcinoma and less differentiated squamous cell carcinoma, in increasing terms of severity. 9 Shear and Pindborg first reported the clinico-pathological description and stated that it was clinically indistinguishable from VC and its diagnosis could be established histologically, they classified VH into a blunt which was broader, flatter and less keratinized verrucous processes and sharp variety which were long, narrow and heavily keratinized. In 2009 reclassification was introduced as plaque and mass type. 8 The features of the mass type variety are associated more with the histopathological criteria. Evidence was put forward that VH and VC may co-exist and that VC may develop from an existing VH, 10 therefore the need of an adequate depth biopsy and histopathological diagnosis for both. VH shows an exophytic growth pattern with epithelial hyperplasia. The epithelial rete are slender, elongated and may show anastomosis. VC has been reported in the literature under a variety of terms, including Buschke–Loewenstein tumor, florid oral papillomatosis, cutis papillomatosis, cutis papillomatosis carcinoides of Gottron, epithelioma cuniculatum,, and carcinoma cuniculatum. 11 The etiology of oral VC is not entirely understood but it is indicative that risk factors include tobacco both inhaled and smokeless forms. 12 VC can develop over or from pre-existing keratotic lesion, OSMF, a premalignant condition, can also produce the development of VC. 6 Histopathologically VH can have dysplasia-like cytologic features that VC does not have. Normal mitotic figures can be seen in the basal or parabasal layer of VC, but not cytological atypia. Although it is recognized that VC can have minimal dysplasia and invasion, the clinical behaviour is similar to VC rather than OSCC and VH can turn into VC. 13 There have been conflicting reports about the metastatic potential of oral VC. According to some authors, an invasive growth exists with disjointed islands and tumor invasion groups cells and thus the ability to metastasis. 14 Usually to detect lymph node metastasis, ultrasonography is the prime choice but the sub-mandibular area shows frequent presence of inflammatory lymphadenopathy which might be difficult to rule out, hence ultrasound guided fine needle aspiration biopsy is must to avert neck dissection of the patient. 15 Adequate modality of treatment being complete surgical excision, both VH or VC should not be disregarded and should be treated as equivalently as OSCC, though radiotherapy as a treatment of modality is contentious as some authors believe that VC is radiosensitive and some propose there maybe radiation induced anaplastic transformation of the cells. 16 VC associated with other potentially malignant disorders maybe a sign of field cancerization and could lead to multiple recurrences, so it is highly indicative that such patients are monitored via regular follow-up. 17
Conclusion
Literature proves that VC can arise from potentially malignant disorders and its differentiation from other verruco-papillary lesions is challenging for the oral diagnostician as they have to be screened periodically and they could be set apart only histologically on the basis of level of rete pegs of the lesion with that of the normal epithelium to it. Hence inclusion of it during excisions is mandatory to arrive at an accurate diagnosis which could enable good outcomes and avert mortality. Frequent presence of malignant foci has been reported, increasing the need of in depth microscopic examination and extensive clinical knowledge.