Introduction
Lichen Planus was initially described by a British physician Wilson Erasmus in the year 1869. It is an autoimmune condition manifested on the skin, hair, eyes, mucous membranes, and nails.1, 2, 3 Those lesions which are present in the oral cavity are referred as oral lichen planus (OLP). Across worldwide among general population, OLP prevalence is about 0.5–2% with females predilection.4 A cross sectional study done among tribal and suburban population of Maharashtra incidence of grinspan syndrome was found to be 1.62%, mainly seen in sub-urban females of 35-50 years.5 Around 53.6% of cutaneous LP patients are associated with OLP.6 Nowadays, Both cutaneous form and oral lichen planus are identified as a chronic muco-cutaneous inflammatory condition which arises from the stratified squamous epithelium. Grinspan et al in 1964, at first reported the prevalence of coexistence of the traid of OLP, diabetes mellitus and hypertension at the Fifth Latin American Dermatology Congress. Later in 1965, Jolly, Powell, Howell and Rick supported the existence of this symptomatic triad.7 In this article, we present a case of symptomatic erosive oral lichen planus with a history of vascular hypertension along with which, diabetes mellitus type II was diagnosed. The co-existence of all three together confirms the case as Grin’s span syndrome.
Case History
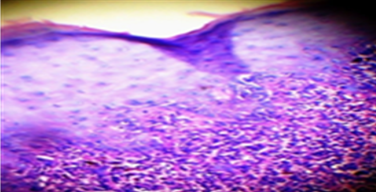
A 46-year-old female patient had come to oral medicine department with the chief complaint of white patches and burning sensation present for past 5 months. The patient history revealed that she had hypertension for a duration of 1 years and under medication for past 6 months amlong (amlodipine) 5 mg. General examination revealed that she had recent loss of weight and excessive thrust for past 4 months. No. other relevant family /personal history. Intra-oral examination revealed, a radiating grayish white lines on the right side (Figure 1) and left side of buccal mucosa (Figure 2) along with areas gingival desquamation was observed in the gingiva (Figure 3). After correlating history & clinical examination, gave a differential diagnosis of oral Lichen Planus and lichinoid reaction. On biochemical and haematological investigation, fasting blood glucose level was found to be 170mg/dl, post prandial blood glucose was 485mg/dl and her HbA1c was 9. Incisional biopsy was done from the right side of buccal mucosa and histopathalogical section of ulceration revealed sub epithelial band of lymphocytic infiltrate, irregular thickening of the epidermis and elongation of the rete ridges with hyperkeratosis and degeneration of basement membrane (Figure 4) which confirmed the diagnosis of oral erosive lichen planus. Type II diabetes mellitus was finally confirmed based on the results of biochemical and haematological investigation.
Figure 1
Intra oral examination showed reticular network of slightly-raised,gray-white line seen on right side buccal mucosa.

On correlating the triad of hypertension, lichen planus and diabetes, the case was finally diagnosed as Grinspan’s syndrome. She was referred to general physician for management of diabetes mellitus for which she was prescribed medications. Oral lesions are treated with Kenacort 0.1% Oral Paste (triamcinolone acetonide 0.1% in aqueous solution), 3 times daily for more than a month. Patient reviewed after 1 month, patient was found to be having a complete relief of burning sensation symptom and white patches did not increase or decrease in size it remains unchanged.
Discussion
Lichen planus has a multifactorial etiology. It is an auto immune disorder which is T cell mediated. The primary event in occurrence of OLP and the factors which influence the susceptibility are not known. Some state a predisposing genetic factor coupled with other factors including, emotional stress, drug induced hypersensitivity, hypersensitivity reactions to dental filling materials, food, etc. OLP has a variable clinical presentation. OLP is of six subtypes namely; reticular, popular, plaque like, erosive, atrophic and bullous. The most prevalent form is the reticular OLP in which Whick-ham striae, an asymptomatic white lace type pattern is seen on the cheek or buccal mucosa.8 Typical lesions of OLP are bilateral in occurrence with posterior buccal mucosa being the most common site. However, it can also be seen tongue, gingiva, retromolar/tuberosity region, vestibule, floor of the mouth and lips. In our case, predominantly gingiva was affected causing desquamation and also buccal mucosa bilaterally. In spite of OLP lesions having distinct clinical presentations, under rare circumstances, a confusing array of patterns may be observed.
A range of 10% - 85% prevalence of DM in OLP patients has been reported.9, 10 Studies state that endocrine dysfunction in DM may lead to an immunological defect, which can result in formation of OLP. A total of 3 cases with apparent drug induced Grinspan’s syndrome with a triad of Oral Lichen Planus, diabetes mellitus and hypertension are reported.11 OLP has been reported in many cases with medical history of diabetes due to the pathogenesis occurring in diabetic patients. Because drugs used to treat hypertenstion and diabetes mellitus may also cause lichenoid type of reaction in the oral cavity, lichenoid reaction causes lesions in the oral cavity which is similar to that of lichen planus hence the name is substantiated as lichenoid reactions, therefore a different hypotheses is put forth Grinspan’s syndrome may be drug induced phenomenon but thankfully gold standard biopsy help to distinguish (iatrogenic) lichenoid reaction from OLP.12
Whereas, this case showed sub epithelial band of lymphocytic infiltrate, irregular thickening of the epidermis and elongation of the rete ridges with hyperkeratosis and degeneration of basement membrane (Fig 4) which confirmed the diagnosis of erosive OLP. Another useful aid in the differentiation of lichenoid and OPL is examination under Immunofluorescent. Gold standard in treatment of OLP is topical and systemic corticosteroids but literature also showed evidence of systemic and topically administered all-trans retinoic acid, Vitamin A, systemic etretinate, and systemic and topical isotretinoin is very effective in the treatment of OLP,13 cyclosporine and photodynamic therapy are some of the other treatment modalities. In our case, we have treated with Kenacort 0.1% Oral Paste (triamcinolone acetonide 0.1% in aqueous solution) along with supplement therapy with vitamins and patient was regularly reviewed after 1 week, and symptoms relieved with medication after1month period.
Grinspan’s syndrome should always be suspected in patients with proven OLP with a history of hypertension, diabetes mellitus. Finally, conclude by quoting the words of William Osler “Mouth is the mirror of the body” oral lesions may have connection with systemic diseases, this case Grins span syndrome is one such finding were oral erosive lichen planus is connected with systemic illness of hypertension and diabetes mellitus.