Introduction
The mandibular molar, premolar, and surrounding gingival teeth are supplied by the Inferior Alveolar Nerve (IAN). The mental nerve emerges from its larger terminal branch from the mental foramen. The mental foramen has three nerve branches coming out of it. The skin of the mental region is innervated by one, while the lower lip, mucous membranes, and gingiva up to the second premolar are innervated by the other two. The canine and incisor teeth are supplied by the incisive branch, which is a continuation of the IAN.1, 2, 3 Any surgical methods involving the posterior mandible must consider the position and direction of the inferior alveolar canal (IAC).4, 5, 6 Therefore, before undergoing any treatment in this location, it is important to take into account the frequent anatomical alterations of the inferior alveolar nerve (IAN) course.7, 6
.Iatrogenic injuries to the inferior alveolar nerve (IAN) are a well-documented side effect of third molar operations, implant placement, osteotomies, or fracture treatment. The terminal section of the IAN as well as the significant variation in the nerve's course, shape, curvature, and direction complicates the regional anatomy. Therefore, it is frequently impossible to determine the exact position of the nerve, preventing adequate preoperative planning.8, 9 The risk of unintentional IAN injury associated with various surgical interventions in the region, such as sagittal split osteotomies or the insertion of fixation screws, may be reduced with a better understanding of the intrabony anatomy of the IAN and its relationship to mandibular molar (MM) anatomical landmarks, particularly with emphasis on the tooth. Numerous studies have highlighted the IAN's unwanted and frequently preventable iatrogenic effects. It has been noted that IAN injury may result in sensory deficits in as many as 8.3% of patients undergoing mandibular ramus harvesting procedures.10, 9 Different radiographs, such as intra oral panoramic radiographs (IOPAR), panoramic radiographs, and cone beam computed tomography, show the mandibular canal. Out of all of these, panoramic radiographs are the most accessible and provide simultaneous bilateral examination.11
The aim of this study is to evaluate the course of inferior alveolar canal (IAC), visibility of the inferior alveolar canal, and IAC origin in Punjabi population (North India).
Materials and Methods
A retrospective study comprised 200 subjects who had undergone panoramic imaging. The Orthopantomographs (OPGs) images were retrospectively evaluated. All samples have been collected from punjabi population and composed of men (83) and women (117) aged 18 to 60. The study group was divided into two subgroups according to age and gender. Age group were classified as follows: <=20, 21-30,30-40,40-50,50-60. Ethical approval was taken for this study. To improve visibility, the image was not digitally altered in any way.
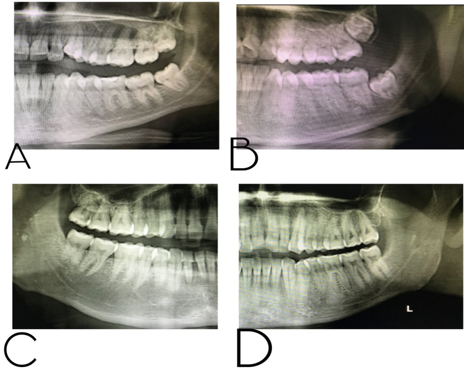
The type of IAC course was diagnosed by visual detection and comparison with references.12 The course of IAC was divided into four categories in the study by Liu et al. based on how it appeared on panoramic radiography, which was defined as Type (1) linear curve (right): a canal that is in contact or in close contact with, or at a maximum distance of 2 mm from, the apex of the first mandibular molars; Type 2 :spoon-shaped curve: canal in close proximity to or in contact with the inferior mandibular cortex, or at a maximum distance of 2 mm; Type (3) oval curve (curved): the location halfway between Type 1 and 2 ; and Type (4) turning curve (angled) 12, 13 (Figure 1)
The distance between the condylar most upper point and the mandibular angle was divided into three equal portions as the upper, middle, and lower parts in order to check the canal entry site. The canal entry point was then classified based on the region in which it was located and noted in the checklist.12, 14 The IAC's appearance and visibility across all images based on the following standards: Type I: Visible (well-defined) superior and inferior borders. Type II: Borders with a visible superior and invisible inferior (partially defined). Type III: Borders with a visible inferior and invisible superior (partially defined). Type IV: Superior and inferior borders that are invisible (not defined.)15
All the OPG’s were taken by Digital Orthopantomograph machine with exposure conditions of 10 mA and 85 kV Max.
These above mentioned factors were evaluated in left and right side of each patient. The recorded data was then complied and entered in the Microsoft excel; and was analyzed by data editor of SPSS software version 20.
Results
This study was performed on 200 digital panoramic images. The age range of our study was 18 to 60 years (Table 1). The mean age of our study was 30.33 (Table 2). Out of 200 radiographs, 41.5 % were of males and 58.5% were of females. (Table 3)
Table 1
Age distribution
|
|
Frequency |
Percent |
|
|
Age |
<=20 |
23 |
11.5% |
|
21-30 |
95 |
47.5% |
|
|
31-40 |
46 |
23.0% |
|
|
41-50 |
28 |
14.0% |
|
|
51-60 |
8 |
4.0% |
|
|
Total |
200 |
100.0% |
|
Table 2
Mean and standard deviation (Age)
|
|
N |
Mean |
Standard Deviation |
Minimum |
Maximum |
|
Age |
200 |
30.33 |
10.37 |
18.00 |
60.00 |
Table 3
Gender distribution of subjects
|
|
Frequency |
Percent |
|
|
Sex |
Male |
83 |
41.5% |
|
Female |
117 |
58.5% |
|
|
Total |
200 |
100.0% |
|
Table 4
Inferior alveolar canal types
Table 5
Visibility of inferior alveolar canal on panoramic radiographs in first molar, second molar and third molar regions.
Table 6
Inferior alveolar canal origin frequency distribution
Table 7
Distribution of inferior alveolar canal types; inferior alveolar canal visibility in the region of first molar, second molar and third molar; inferior alveolar canal origin among males and females on right side.
Table 8
Distribution of inferior alveolar canal type; inferior alveolar canal visibility in the region of first molar, second molar and third molar; inferior alveolar canal origin among males and females on left side.
The most common type of canal on right and left side was curved type (84.5% on the right side and 80.5% on the left side), and the less common was Angled type (2.5% on the right side and 3% on the left side).
On panoramic radiographs, the percentage of the Inferior alveolar nerve canal that was invisible in the first molar region on the Right Side was 30%, partially visible in 53.0%, and clearly visible in 17%., whereas on the left side, it was invisible in 27%, partially visible in 64% and clearly visible in 13.5%.
In second molar region, it was invisible in 16%, partially visible in 41.5% and clearly visible in 42.5% on right side. It was invisible in 13.5%, partially visible in 49% and clearly visible in 37.5% on left side.
In the region of the third molar, on Right side, the Inferior alveolar nerve canal was partially visible in 1.5% of cases, clearly visible in 96.5%, and invisible in 2%; whereas on left side, it was clearly visible in 97%, partially visible in 5%and invisible in 2.5%. (Table 5)
The findings showed that the entrance point of the canal was located in the middle third area of the ramus in 87% of cases on the right side and 90% cases on the left side, and that the entrance point of the canal in the lower third area was 7.5% on the right side and 3.5% on the left side. (Table 6)
Distribution of Inferior Alveolar Canal Types; Inferior Alveolar Canal Visibility in the region of First Molar, Second Molar And Third Molar; Inferior Alveolar Canal origin among Males And Females on Right and Left Side are given in Table 7, Table 8 below.
Discussion
The regional anatomy is made more challenging by differences in the IAN's course, shape, curve, and orientation. The majority of prior descriptions of the IAN anatomy were inaccurate. As a result, there is a higher risk of unintentional IAN injury with different surgical operations in the region.16 Since panoramic radiography provides a comprehensive perspective of the teeth and oral structures; it is frequently employed in dental practice. In terms of the IAN, it is typically easily visible, allowing the practitioner to assess the risk of IAN injury during invasive operations. However, this 2D technique does not show the IAN itself and lacks 3D information.17, 18 In this study, the course of Inferior alveolar canal was observed along with its entry and visibility in mandibular posterior region on both the sides of mandible. We followed the classification given by Liu et al. who classified it into Type (1) linear curve (right), Type 2 :spoon-shaped curve, Type (3) oval curve (curved) and Type (4) turning curve (angled).1, 2 In our study, the most common type of canal on right and left side was Oval Curve type (84.5% on the right side and 80.5% on the left side), and the less common was Angled type (2.5% on the right side and 3% on the left side). However, in the study conducted by Jung YH et al.,19 it was observed that the most common course of Inferior Alveolar Canal was an elliptic curve (64.7%), and this was followed by linear (22.9%) and spoon-shaped curves (6.9%). In the study conducted by Liu et al., elliptic curves were the most prevalent (48.5%), and spoon-shaped curves were the next most prevalent course (29.3%).13
In our study, Clear Visibility of Inferior Alveolar Canal was more on distal regions of the canal on the both the sides of the mandible. On the right side, in the first molar region, mandibular canal was invisible in 30%, partially visible in 53.0%, and clearly visible in 17%. In second molar region, it was invisible in 16%, partially visible in 41.5% and clearly visible in 42.5. In the region of the third molar, it was partially visible in 1.5% of cases, clearly visible in 96.5%, and invisible in 2%. On the left side, in the first molar region, it was invisible in 27%, partially visible in 64% and clearly visible in 13.5%, whereas it was invisible in 13.5%, partially visible in 49% and clearly visible in 37.5% in the second molar region. It was clearly visible in 97%, partially visible in 5%and invisible in 2.5%in third molar region. Similar results were observed in the study conducted by Abhijeet Alok et al.11 where when the distal region of the mandibular canal was approached, visibility of the canal was also increased. In the area surrounding the third molar, the mandibular canal was fully visible in 47% of sites, somewhat visible in 51.7%, and invisible in just 1.3%. In 22.6% of sites in the first mandibular area, 11.8% in the second molar regions, and 1.3% in the third molar regions, the mandibular canal was undetectable.
In 32% of the sites in the molar region that were examined, according to Naitoh et al., the canal was completely invisible on panoramic images.20
In our present study, it was found that the entrance point of the canal was located in the middle third area of the ramus in 87% of cases on the right side and 90% cases on the left side, and that the entrance point of the canal in the lower third area was 7.5% on the right side and 3.5% on the left side. Similar findings were revealed in the study conducted by in the study conducted by Ali Derafshi et al.21 where the entrance point of the canal was in the middle third area of the ramus in 97.15% of cases, and that the entrance point of the canal in the lower third area was not visible in any of the images. To avoid any complications, it is important to have the correct knowledge of course, visibility and entrance point of Inferior Alveolar Canal is important. Therefore, this study was conducted to evaluate the course of inferior alveolar canal (IAC), visibility of the inferior alveolar canal, and Inferior Alveolar Canal origin in Punjabi population (North India).
Conclusion
This study was done to evaluate course, visibility, and entry point of Inferior Alveolar Nerve Canal on the Orthopantomograph. In our present study, the most common type of canal on right and left side was Curved type, and the less common was Angled type. The entrance point of the canal was located in majority in the middle third area of the ramus on left and right side of the mandible. Clear Visibility of Inferior Alveolar Canal was more on distal regions of the canal on the both the sides of the mandible.