- Visibility 57 Views
- Downloads 10 Downloads
- DOI 10.18231/j.jdp.2023.015
-
CrossMark
- Citation
Use of laser in the management of leukoplakia and oral lichen planus - A systematic review
Introduction
According to the World health organization (WHO), cancer is the second most common cause of death in developing countries. Oral cancer accounts for about 3–4% of all cancers. Potentially malignant oral lesions (PMOLs) are clinically and histologically distinct lesions preceding towards malignant changes.[1] According to Warnakalasurya, in 2005, this term has been changed to “Oral potentially malignant disorder.” WHO enlisted PMDs include: Leukoplakia, Erythroplakia, Proliferative Verrucous Leukoplakia, Oral Lichen planus, Oral Submucous Fibrosis, Actinic Cheilitis, Palatal lesion of reverse smoking, Oral Lupus Erythematous, Dyskeratosis Congenital and Oral Epidermolysis Bullosa. Amongst all leukoplakia and oral lichen planus are the most common potentially malignant disorders. [2]
Leukoplakia (LP)
“In 2005, WHO defined leukoplakia as “a white plaque of questionable risk having excluded other known diseases or disorders that carry no increased risk for cancer”.
Numerous etiological factors have been implicated with leukoplakia, such as tobacco, alcohol, viral infections, candidiasis, and chronic irritation associated with dentures and cheek biting.[3] These lesions are reported to have a potential for malignant transformation to carcinomas with a transformation rate ranging from 0.7% to 6%. The prevalence of leukoplakia in India varies from 0.2% to 4.9%. Men are affected more frequently than women, in the age range of 35-45 years. The most common sites are the buccal mucosa, alveolar mucosa, and lower lip. Lesions in the floor of the mouth, lateral border of the tongue, and lower lip are most likely to show dysplastic or malignant changes. LP is classified into two main types: homogeneous type which appears as a flat white lesion and non-homogeneous type which includes speckled, nodular, and verrucous LP. [4]
The first line management of LP begins with the elimination of etiological factors. Conservative treatment includes the use of chemopreventive agents such as vitamins (vitamins A, C, E), fenretinide (Vitamin A analog), carotenoids (beta-carotene, lycopene), bleomycin, protease inhibitor, anti-inflammatory drugs, green tea, curcuma, etc. Surgical treatment includes conventional surgery, electrocoagulation, cryosurgery, and laser surgery (excision or evaporation). Cryosurgery is simple, safe, time-tested, and an effective modality of treatment for LP. Light amplification by stimulated emission of radiation (LASER) provides a bundle of options over conventional surgery as they provide the advantage of precise excision, homeostasis, reduced postoperative swelling and pain. [5]
Oral lichen planus (OLP)
Oral Lichen planus (OLP) is a chronic inflammatory mucocutaneous disease of unknown etiology in which apoptosis of basal keratinocytes is induced by CD8 +T cells. It usually affects the middle and old age population with the female: male ratio being 2:1 and the age range documented is between 30–60 years.[6]
Typically, the disease presents with multiple lesions with the bilateral symmetrical distribution. Andreasen’s classification divides oral lichen planus (OLP) into six clinical forms: reticular, papular, plaque-like, atrophic (erythematous), erosive-ulcerous, and bullous-erosive.[7]
At the early disease stage treatment is usually aimed to abolish the symptoms and extend the periods of remission while complete disease eradication cannot be achieved by any approach. Corticosteroids, despite their various adverse effects like thinning of the oral mucosa, secondary candidiasis, and tachyphylaxis is considered the gold standard in the treatment of OLP. Topical calcineurin inhibitors such as tacrolimus; topical and systemic retinoids such as tretinoin and immunosuppressants such as azathioprine have been considered as an alternative to corticosteroids. The alternative promising non-pharmacological modality that should be considered is LASER phototherapy.
Laser
LASER is a novel prophylactic and therapeutic device that produces light energy through a process of optical amplification generating a high-intensity parallel beam of monochromatic electromagnetic radiation. Dental laser are based emission wavelengths, for various clinical application, which span from the visible to the far infrared portions of the electromagnetic spectrum (approximately 400-10,600 nm).
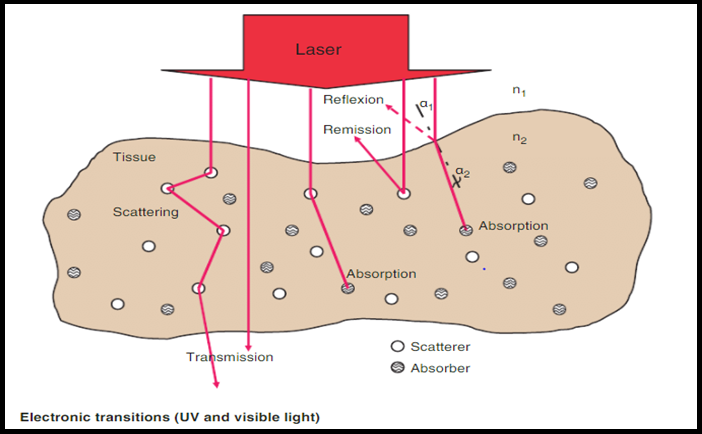
Biological interation of LASER
The light energy produced by a laser can have four different interactions with a target tissue reflection, transmission, scattering, and absorption. When a laser is absorbed, it elevates the temperature and produces photochemical effects depending on the water content of the tissues. When a temperature of 100°C is reached, vaporization of the water within the tissue occurs, a process called ablation. At temperatures below 100°C, but above approximately 60°C, proteins begin to denature, without vaporization of the underlying tissue. Conversely, at temperatures above 200°C, the tissue is dehydrated and then burned, resulting in an undesirable effect called carbonization. Absorption requires an absorber of light, termed chromophores, which have a certain affinity for specific wavelengths of light. The primary chromophores in the intraoral soft tissue are melanin, hemoglobin, and water, whereas in the dental hard tissues, water and hydroxyapatite. [8]
Advantages of LASER include
Haemostatic effect to maintain bloodless operative field, accurate removal of lesion, minimal damage to adjacent tissue, reduction in acute inflammatory reaction which alleviates post operative pain, excellent wound healing, minimal wound contraction and oral dysfunction.
The only disadvantage of using LASER as a treatment modality is the destruction of the removed tissue that leads to limited histopathological analysis and delayed epithelial regeneration when compared to surgical excision with suture. (Ishii et al., 2004; Vivek et al., 2008; Hamadah et al., 2009).
This systematic review aims to evaluate and compare the efficacy and effectiveness of LASER in the management of LP and OLP so as to restrict the progression of these to malignancy.
Materials and Methods
The aim of this research was to compare the effectiveness of LASER (light amplification by stimulated emission of radiation) on the management of leukoplakia and lichen planus.
Objectives were to understand the effectiveness of laser in disease remission in leukoplakia and oral lichen planus, incidence of recurrence of leukoplakia post LASER therapy and the rate of malignant transformation in leukoplakia treated with LASER.
Research question
Is LASER an effective treatment modality for oral leukoplakia and oral lichen planus?
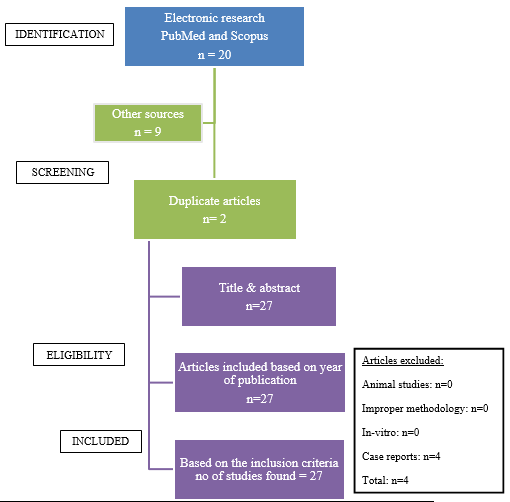
SEARCH STRATEGY: Electronic databases (PubMed, Scopus) were searched, using various combinations of the following keywords: potentially malignant disorders, leukoplakia, oral lichen planus, and LASER therapy from the year 2002 to 2021. Owing to the heterogeneity of data, no statistical analyses were conducted.
Results
Since the reviews published for the management of PMDs like LP and OLP are few in number and does not carry homoginicity in its data astatistical analysis could not be conducted. Nevertheless, an observational tabulation has been done for the same.
|
Author/year |
Type of laser modality used |
Recurrence rate |
Malignant transformation |
|
Ishii J et al (2004) [9] |
Laser |
29% shows recurrence, |
3.4 % shows the malignant transformation |
|
Meister J et Al. (2010) [10] |
liquid core light guides |
No reoccurrence |
Not observed |
|
Shafirastein G et al. (2011) [11] |
pulsed dye laser |
(41%) had more than 75% regression (53%) had more than 25% regression (partial response) |
Not observed |
|
Huang z et al. (2014) [12] |
CO2 laser therapy |
10% shows reoccurrence |
Not observed |
|
Singh KP et al. (2015) [13] |
carbon dioxide laser |
9.10% recurrence rate |
2.27% malignant transformation |
|
Natekar M et al. (2017) [14] |
cryosurgery, diode, and CO2 laser surgery |
Not observed (Between diode and co2 laser, the pain was significantly higher in co2 laser.) |
Not observed |
|
Lim JY et al. (2018) [15] |
CO2 versus anxiolytic laser |
21%) showed recurrent leukoplakia treated with both modalities. |
(7%) showed histologic grade progression with co2 laser and 5%shows disease progression with angiolytic laser. |
|
Jurczyszyn K et al. (2020) [16] |
Er: YAG Dental Laser. |
Recurrence occurred in 34% of lesions |
Not observed |
|
Das S et al. (2021) [17] |
Nd: YAG laser |
Recurrence was noted in 2 patients but following the second application, there was no recurrence over the period of further follow-up. |
No malignant transformation after the treatment |
|
Author/year |
Type of laser used |
Inference |
|
Cafaro A et al. (2010) [18] |
Low-level laser therapy (LLLT) with pulsed diode laser (GaAs). |
Reduction in lesion size and pain |
|
Cafaro A et al. (2014) [19] |
(GaAIAs) diode laser |
Significant reduction in clinical scores of pain |
|
Al-Maweri A S et al (2017) [20] |
(LLLT) |
Significant reduction in clinical scores of pain |
|
Khater M, Fathia M (2019) [21] |
Nd: YAG laser |
Significant reduction in pain. |
|
Slebioda Z, Dorocka-Bobkowska B(2020) [22] |
LLLT |
Accelerated healing process and pain reduction. |
Discussion
The treatment of PMD’s, like LP and OLP, represents therapeutic challenges. Recent use of various LASER therapies have gained popularity due to its advantages over conventional methods such as drug therapy, conventional surgery, electro-coagulation, and cryosurgery. The numerous advantages of laser are its haemostatic effect, precise removal of the lesion, minimal adjacent tissue damage, excellent wound healing, and minimal oral dysfunction.
Ishii J et al., (2003),[3] in their review on oral leukoplakia patients treated with laser, observed that there is 29.3% recurrence and 1.2% malignant transformation after the use of laser. They concluded that non-homogenous leukoplakia on non-keratinized epithelia has a high risk for malignant transformation, therefore should be excised after detecting abnormal epithelia. In the year 2014, Huang z et al.[12] conducted a retrospective study and evaluated the safety and advantages of using carbon dioxide (CO2) laser in the treatment of oral mucosal lesions. None of the patients had postoperative infections, and the wound showed uneventful healing in 1 year of follow-up. Two patients showed recurrence which healed completely on re-operation. The second group was the control group which included twenty patients with lesions removed using the traditional scalpel. The authors concluded that the application of CO2 laser in the treatment of oral mucosal lesions has the advantages of reduced bleeding, a clear view during surgery, and a shorter operative time.[12] Previously authors have compared different types of lasers in the treatment of OL. One such study was conducted by Natekar M et al.,[14] in 2017, who compared diode laser, CO2 laser, and cryosurgery, They observed that pain was minimal, haemostasis was favorable, and wound healing was good with no post-operative complications when diode laser was used while the pain was significantly higher in the CO2 laser.[14] Another study was done by Das S et al. [17] in the year 2021, to evaluate the role of Nd: YAG laser in the management of oral leukoplakia and he investigated postoperative complications along with the long-term prognosis of the disease. The authors concluded that Nd: YAG laser was found to be effective in ablating leukoplakia with no incidence of infection, paresthesia or anasthesia. These findings are in concurrence with previous studies. [17] On the contrary, Singh KP et al.,[13] in the year 2015, reported the recurrence rate and malignant transformation rate of oral leukoplakia after carbon dioxide laser treatment as 9.10% and 2.27% respectively.
Studies were also conducted on laser intervention in the treatment of oral lichen planus. [13] In the year 2010,Cafaro A et al.[18] conducted a prospective cohort study to detail the efficacy of LLLT for the management of OLP unresponsive to standard therapy. The authors concluded by highlighting that LLLT could be a possible treatment for patients with unresponsive OLP. A systemic review was done by Maweri AS et al.[20] (2017), to assess the efficacy of low-level laser therapy in the treatment of symptomatic OLP. The results of the included studies confirmed that LLLT was effective in the management of symptomatic OLP and can be used as an alternative to corticosteroids. In yet another a study was conducted by Slebioda Z, Dorocka-Bobkowska B[22] in 2020, with an aim to discuss the mechanism of action and the biological effects of LLLT. The authors critically reviewed and summarized recent clinical reports on the management of RAS and OLP. They stated that LLLT is of interest as a novel treatment modality. Most of the studies demonstrated the beneficial effect of LLLT in accelerating the healing process and pain reduction. [22] In the year 2018, Karandeep S A et al. [23] conducted an observational study with an aim to evaluate the efficacy of diode laser in the management of homogenous oral leukoplakia (OL) and reticular oral lichen planus (OLP). None of the subjects reported of pain, swelling, or bleeding and it was noted that all the areas treated with laser had healed without scarring with no signs of recurrence. Fibrosis was seen in two male patients and one female patient treated for OL and OLP respectively.
Conclusion
This systemic review was done with an intent to evaluate the effectiveness of LASER as a treatment modality for leukoplakia and oral lichen planus. Various conventional treatments have been reported such as excisional surgery, electro-coagulation, cryosurgery, and medication. This systemic review concludes that LASER is one of the most effective treatment modalities as it has various advantages over conventional treatment such as shorter operative time, reduced volume of blood loss, minimal adjacent tissue damage, excellent wound healing, and minimal oral dysfunction. The overall malignant transformation rate and recurrence rate after conventional surgery is 3-11% and 13-42% respectively, whereas with laser there is a significant decline in the malignant transformation which is 1.2%, and recurrence rate which is 29.3%.
This systematic review has conducted on the efficiency of laser in the management of LP and OLP, it was observed that laser stood as a supreme treatment modality. It was observed that laser overcame the limitations of both conventional and surgical management documented till date when evaluated on the parameters of remission, recurrence, and malignant potential. In OLP LLLT is used as an effective alternative to corticosteroid and in recalcitrant cases. Therefore, LASER is a preferred modality as it non-invasive, painless, bloodless, and bio stimulatory treatment modality.
Source of Funding
None.
Conflict of Interest
None.
References
- FW Mello, AFP Miguel, K L Dutra, AL Porporatti, S Warnakulasuriya, ENS Guerra. Prevalence of oral potentially malignant disorders: A systematic review and meta-analysis. J Oral Pathol Med 2018. [Google Scholar]
- SC Sarode, GS Sarode, JV Tupkari. Oral potentially malignant disorders: Precising the definition. Oral Oncol 2012. [Google Scholar]
- J Ishii, K Fujita, T Komori. Laser surgery as a treatment for oral leukoplakia. Oral Oncol 2003. [Google Scholar]
- N Aggarwal, S Bhatefa. Leukoplakia- Potentially Malignant Disorder of Oral Cavity -a Review”. Biomed J Sci Tech Res 2018. [Google Scholar]
- P Ioannina, G Carmen, C Elena. Serban T- Oral Leukoplakia - An Update”.MAEDICA-a. J Clin Med 2014. [Google Scholar]
- PB Sugerman, NW Savage, LJ Walsh, ZZ Zhao, XI Zhou, A Khan. The pathogenesis of oral lichen planus. Crit Rev Oral Biol Med 2002. [Google Scholar]
- S Gupta, M K Jawanda. Oral Lichen Planus: An Update on etiology, pathogenesis, clinical presentation, diagnosis, and management. Indian J Dermatol 2015. [Google Scholar]
- S K Verma, S Maheshwari, R K Singh, P K Chaudhari. Laser in dentistry: An innovative tool in modern dental practice. Natl J of Maxillofac Surg 2012. [Google Scholar]
- M Natekar, HP Raghuveer, DK Rayapati, ES Shobha, NT Prashanth, V Rangan. A comparative evaluation: Oral leukoplakia surgical management using diode laser, CO2 laser, and cryosurgery. J Clin Exp Dent 2017. [Google Scholar]
- JH Lim, YM Park, M Kang, SJ Lee, K Baek, J Na. Angiolytic laser stripping versus CO2 laser micro flap excision for vocal fold leukoplakia: Long-term disease control and voice outcomes. PLoS ONE 2018. [Google Scholar] [Crossref]
- J Meister, R Franzen, G Eyrich, J Bongartz, N Gutknecht, P Hering. First clinical application of a liquid-core light guide connected to an Er:YAG laser for oral treatment of leukoplakia. Lasers in Med Sci 2010. [Google Scholar] [Crossref]
- S Das, S Mohammad, V Singh, S Gupta. Neodymium: Yttrium aluminum garnet laser in the management of oral leukoplakia: A case series. Contemp Clin Dent 2015. [Google Scholar]
- K P Singh, Ghm Mir, U Jeelani, S Gupta, P Koul, P Kalsotra. Carbon Dioxide Laser surgery in Management of oral leukoplakia. Int J Contem Med Res 2016. [Google Scholar]
- Z Huang, Y Wang, Q Liang, L Zhang, D Zhang, W Chen. The application of a carbon dioxide laser in the treatment of superficial oral mucosal lesions. J Craniofac Surg 2015. [Google Scholar]
- J Ishii, K Fujita, S Munemoto, T Komori. Management of oral leukoplakia by laser surgery: relation between recurrence and malignant transformation and clinicopathological features. J Clin Laser Med Surg 2004. [Google Scholar]
- G Shafirstein, A Friedman, E Sieqel, M Moreno, W Baumler, C Y Fan. Using 5-Aminolevulinic Acid and Pulsed Dye Laser for Photodynamic Treatment of Oral Leukoplakia. Arch Otolaryngol-Head Neck Surg 2011. [Google Scholar]
- K Jurczyszyn, M Kozakiewicz. Application of Texture and Fractal Dimension Analysis to Estimate Effectiveness of Oral Leukoplakia Treatment Using an Er:YAG Laser-A Prospective Study. Materials (Basel) 2020. [Google Scholar] [Crossref]
- Z Ślebioda, BD Bobkowska. Low-level laser therapy in the treatment of recurrent aphthous stomatitis and oral lichen planus: a literature review. Postepy Dermatol Allergol 2020. [Google Scholar]
- A Cafaro, G Albanese, P G Arduino, C Mario, G Massolini, M Mozzati. Effect of Low-Level Laser Irradiation on Unresponsive Oral Lichen Planus: Early Preliminary Results in 13 Patients. Photomed Laser Surg 2010. [Google Scholar] [Crossref]
- A Cafaro, P Arduino, G Massolini, E Romagnoli, R Broccoletti. Clinical evaluation of the efficiency of low-level laser therapy for oral lichen planus: a prospective study. Lasers Med Sci 2014. [Google Scholar]
- SA Al-Maweri, B Kalakonda, WA Al-Soneidar, HM Al-Shamiri, MS Alakhali, N Alaizari. Efficacy of low-level laser therapy in the management of symptomatic oral lichen planus: a systematic review. Lasers Med Sci 2017. [Google Scholar]
- MM Khater, FM Khattab. Efficacy of 1064 Q switched Nd: YAG laser in the treatment of oral lichen planus. J Dermatolog Treat 2019. [Google Scholar]
- K Arora, R Bansal, S Mohapatra, A Verma, S Sharma, S Pareek. Prevention of Malignant Transformation of Oral Leukoplakia and Oral Lichen Planus Using Laser: An Observational Study. Asian Pac J Cancer Prev 2018. [Google Scholar]
