- Visibility 188 Views
- Downloads 12 Downloads
- DOI 10.18231/j.jdp.2023.026
-
CrossMark
- Citation
To correlate interlabial gap, lip morphology and lip strain in various skeletal malocclusions in distt solan population – A cephalometric study
Introduction
One of the goals of orthodontic treatment is to create a beautiful, balanced face. A therapeutic strategy to normalise the face characteristics of a specific person can be developed using knowledge of the soft tissues and their normal ranges (Sandra et al. 2008). The improvement in the patient's facial appearance, including the soft tissue profile, is frequently correlated with the success of orthodontic therapy by (Bass, 2003).[1], [2]
The placement of teeth in accordance with recognised cephalometric parameters does not guarantee that the soft tissue that lies above it will drape harmoniously. According to research, soft tissue doesn't always react well to hard-tissue retraction. Profile components have also been used to analyse the soft-tissue profile. The line through the nasal floor and these profile elements' angular tilt allow for a more complex study of the vertical and anterior posterior components of the facial profile.
Several line analyses have been suggested for evaluating lip posture and the esthetic quality of the profile.’ Worthy of mention is Rickett’s “E” line,’ which is influenced a great deal by growth of the nose. Steiner’s “S” linez eliminates half of the change in integumental profile due to growth of the nose. Holdaway’s “H” line has the advantage of removing the influence of nasal growth in the evaluation of lip posture. Merrifield’s “Z” angle’ expresses the full extent of lip protrusion in malocclusions. [3]
The numerous analyses available for evaluating soft-tissue profile and the lack of standardization in research methods make it difficult to draw comparisons between results reported by various researchers.
Different methods can be used to evaluate soft tissue morphology, which is an essential tool in clinical practice and research. Radiographic techniques are the most effective and are hence most frequently utilized. They include measuring reference points and landmarks, as well as a comprehensive and analytical assessment of the subject's particular craniofacial features (Ricketts, 1981). [4]
In orthodontic treatment, various analyzes are carried out to establish a case diagnosis which is then also useful in helping to develop the best treatment plan that can result in a good dentition, attractive smile and attractive profile. These three factors are part of a number of other factors that influence the aesthetic quality of a person’s appearance. Cephalometric analysis can be used to determine the status of these three factors through several measurements of related parameters.
In order to enhance their appearance, patients who seek orthodontic treatment (Kuhn et al., 2016). The lip shape is one of the most significant elements determining the aesthetic profile, with race, ethnicity, gender, age, society, and psychology being some of the other aspects that have an impact on the aesthetic standard of the facial profile (Solem et al., 2013; Alkadhi et al., 2019). In orthodontic therapy, it frequently involves incisor position management to create a change in lip morphology.
In the case of bimaxillary protrusion, incisor retraction is crucial in orthodontic therapy because it can, to some extent, predict the changes in the soft tissue of the lip that take place after premolar extractions (Solem et al.). The specific link between the sagittal change in incisor position and the reaction of the upper lip, however, is up for debate (Leonardi et al., 2010; Konstantonis, 2012; Alkadhi et al.). For the goal of making a clinical diagnosis and determining a course of treatment, information regarding pertinent human groups or races is crucial. Particularly in orthodontics, maxillofacial surgery, and prosthodontics where arch shape can be significantly adjusted, ethnic distinctions in facial profile and skeletal features should be considered during treatment (Burris and Harris, 2007). [5]
Aim and Objectives
To corelate lip morphology, lip strain and interlabial gap in various skeletal malocclusions in dist solan population.
Materials and Methods
The study was conducted on 50 pretreatments lateral cephalograms of individuals who reported to or have undergone fixed orthodontic treatment in the department of Orthodontics and Dentofacial Orthopedics, Bhojia Dental College and hospital. Inclusion criteria icluded patient with Skeletal Class I (ANB = 2±2º) and patients with skeletal Class II (ANB >4º) with overjet more than 4 mm, complete permanent dentition irrespective of third molar and good quality radiographs. Exclusion Criteria included Previous history of orthodontic treatment, missing, supernumerary or impacted teeth and Craniofacial abnormality. The sample was divided into 2 groups: Group I (skeletal Class I, N=25) and Group II (skeletal Class II, N=25) on the basis of their ANB angle.
|
Group I |
Group II |
|
Skeletal class I (N = 25) ANB=(2±2°) |
Skeletal class II (N = 25) ANB=(≥4°) |
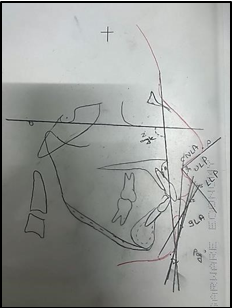
All the cephalograms obtained were traced by the same operator.various landmarks and parameters were identified and marked ([Table 2], [Table 3], [Table 4], [Table 5]) ([Figure 2], [Figure 3])
|
Landmark |
Descriptions |
|
Pronasale (prn) |
Most prominent or anterior projection point of nose |
|
Subnasal (sn) |
Junction of columella and upper cutaneous lip |
|
Pogonion (pg) |
Most anterior point of soft-tissue chin |
|
Labiale superius (ls) |
The mucocutaneous junction or midpoint of the upper vermilion line |
|
Labiale inferius (li) |
The mucocutaneous junction or midpoint of the lower |
|
Columella (C) |
The most anterior and highest part of the columella |
|
B point (B) |
The deepest part between labialis inferius and pogonion |
|
Distant Chin (Dc) |
The most distant point of the chin from the tragion |

|
Planes |
Defination |
|
SN |
A line joining Sella and Nasion representing Anterior Cranial base |
|
FH |
Line passing trough the porion and crosses orbitale |
|
H Line |
Tangent to the chin point and the upper lip |
|
S Line |
Line drawn from Midpoint between subnasale and pronasale to soft tissue pogonion |
|
B line |
Line drawn from soft tissue subnasale to soft tissue pogonion |
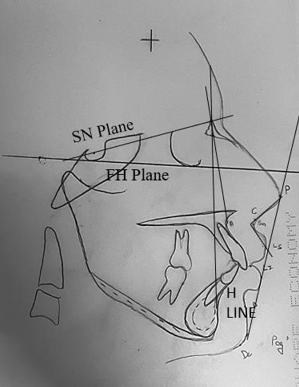
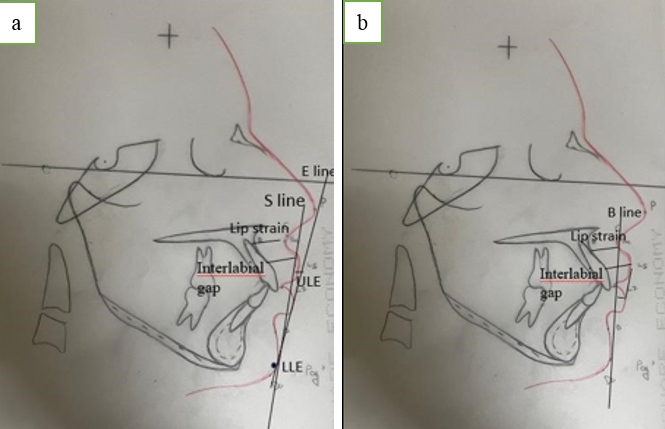
Various angular and linear parameters were measure to record lip strain, lip morphology and interlabial gap.([Table 4], [Table 5]) ([Figure 3], [Figure 4]a,b)
|
Parameters |
Defination |
|
Interlabial Gap |
Distance between Labriale Supeius (LS) and Labiale Inferius (LI) |
|
Lip Strain |
Upper-lip thickness (ULT) - The line between the labiale superius and the labial surface of the upper incisor |
|
|
Lower lip thickness (LLT) The line between the labiale inferius and the labial surface of the lower incisor |
|
Lip Morphology |
ULE- Upper lip to E line LLE -Lower lip to E line |
|
|
ULS - Upper lip to S line LLS - Lower lip to S line |
|
|
LLH Lower lip to H line |
|
|
ULB- Upper lip to B line LLB -Lower lip to B line |
|
Parameters |
Description |
|
Nasolabial angle (NLA) |
Angle formed by profile points columella breakpoint, subnasale and labiale superius |
|
inferior labial angle (ILA) |
Angle formed by profile points labialis inferior, soft tissue B point and pogonion |
|
Z angle (Z) |
Inner inferior angle formed by the intersection of the Frankfort horizontal plane and profile line |
|
Upper lip protrusion angle (ULPA) |
Angle formed between line connecting soft tissue pogonion and the most protrusive upper lip |
|
Lower lip protrusion angle (LLPA) |
Angle formed between line connecting soft tissue pogonion and the most protrusive lower lip |
Statically analysis
The value so obtained were subjected to statistical analysis using SPSS software.
Results
Pre treatment lateral cephalograms of 50 patients who underwent orthodontic treatment were included in the study. They were divided into 2 groups i.e: Group I (Skeletal Class I,N=25) and Group II (Skeletal Class II,N=25). Various linear and angular parameters were recorded for both the groups. When the means of the linear parameters were analysed by compariung group I and group II it was found that there were no statistically significant difference in UL-E (p=1.00), LL-E(p=0.45), UL-S(p=0.51), LL-S(p=0.36) ,ULB(p=0.63), LL-B(p=0.44) ,LL-H(0.71), UL- T(p=0.58), LL-T(p=o.47). On the contrary statistically significant difference was found in interlabial gap (LS-LI) (p=0.00) as depicted in [Table 6].
|
Linear parameters |
Skeletal class I (Mean ±SD) |
Skeletal class II (Mean ±SD) |
F value |
P value |
|
LS-LI |
4.24 ± 1.20 |
5.68 ± 1.37 |
.544 |
0.00* |
|
UL-E |
1.38 (±1.66) |
1.48 (±1.29) |
0.025 |
1.00 |
|
LL-E |
3.04(±1.81) |
3.48 (±2.31) |
0.343 |
0.45 |
|
UL-S |
2.12(±1.53) |
2.44(± 1.87) |
1.044 |
0.51 |
|
LL-S |
3.68(±1.86) |
4.20 (±2.12) |
0.648 |
0.36 |
|
UL-B |
2.28 (± 1.62) |
2.08 (±1.28) |
0.433 |
0.63 |
|
LL-B |
3.96 (±1.81) |
3.56 (± 1.82) |
0.002 |
0.44 |
|
LL-H |
3.72 (±1.72) |
3.92 (±2.10) |
0.166 |
0.71 |
|
LS |
2.04 (±1.01) |
2.12 (±0.97) |
0.145 |
0.77 |
When the means of the angular parameters were analysed by compariung group I and group II it was found that there were no statistically significant difference in NLA (p=0.19), ILA(p=0.71), Z angle(p=0.74),ULPA(p=0.23),LLPA(p=0.76), as depicted in [Table 7].
|
Parameter |
Skeletgal class I (Mean ±SD) |
Skeletal class II (Mean ±SD) |
F value |
P value |
|
Nasolabial angle (NLA) |
92.92 (±13.19) |
97.64(±12.19) |
.009 |
0.19 |
|
inferior labial angle (ILA) |
112.32(±16.90) |
110.48(±18.05) |
.130 |
0.71 |
|
Z Angle |
79.88 (±7.67) |
79.12 (±8.59) |
.959 |
0.74 |
|
ULPA (Upper lip Protrusion) |
98.36(±18.61) |
92.40(±16.24) |
.856 |
0.23 |
|
LLPA (Lower lip Protrusion) |
96.88(±15.13) |
2.12 (±0.97) |
.123 |
0.76 |
When lip strain, lip morphology and interlabial gap parameters were correlated in skeletal Class I malocclusion using pearson correlation, it was found that there was positive correlation of UL-E with LL-E,UL-S Line, LL-S,UL-B, LL-B (p=0.00*), LL-E with UL-S, LL-S line, UL-B, LL-B, LL-H (p=0.00*), UL-S with UL-B, LL-B (p=0.00*), LL-S with UL-B, LL-B(p=0.00*),LL-H (p=0.01*), UL-B with LL-B(p=0.00*), LL-B with LL-H (0.00*), LL-H with Z angle (p=0.01*), NLA with ULPA (p=0.03*), ULPA with LLPA(0.01*). as depicted in [Table 8].
|
Parameters |
LS- LI |
UL-E |
LL-E |
UL-S |
LL-S |
UL-B |
LL-B |
LL-H |
NLA |
ILA |
Z ANGLE |
ULPA |
LLPA |
|
LS-LI |
0 |
0.70 |
0.72 |
0.74 |
0.86 |
0.63 |
0.53 |
0.36 |
0.14 |
0.28 |
0.71 |
0.73 |
0.33 |
|
UL-E |
0.70 |
0 |
0.00* |
0.00* |
0.00* |
0.00* |
0.00* |
0.38 |
0.24 |
0.33 |
0.61 |
0.51 |
0.85 |
|
LL-E |
0.72 |
0.00* |
0 |
0.00* |
0.00* |
0.00* |
0.00* |
0.00* |
0.79 |
0.37 |
0.73 |
0.12 |
0.62 |
|
UL-S |
0.74 |
0.00* |
0.00* |
0 |
0.00* |
0.00* |
0.00* |
0.41 |
0.15 |
0.74 |
0.18 |
0.45 |
0.85 |
|
LL-S |
0.86 |
0.00** |
0.00** |
0.00** |
0 |
0.00** |
0.00** |
0.01* |
0.67 |
0.79 |
0.74 |
0.18 |
0.38 |
|
UL-B |
0.63 |
0.00** |
0.00** |
0.00** |
0.00** |
0 |
0.00** |
0.62 |
0.58 |
0.57 |
0.44 |
0.24 |
0.93 |
|
LL-B |
0.53 |
0.00** |
0.00** |
0.00** |
0.00** |
0.00** |
0 |
0.00** |
0.94 |
0.47 |
0.34 |
0.40 |
0.49 |
|
LL-H |
0.36 |
0.38 |
0.00* |
0.14 |
0.01* |
0.62 |
0.00* |
0 |
0.70 |
0.55 |
0.01* |
0.85 |
0.20 |
|
NLA |
0.14 |
0.29 |
0.79 |
0.15 |
0.67 |
0.58 |
0.94 |
0.70 |
0 |
0.81 |
0.68 |
0.03* |
0.09 |
|
ILA |
0.28 |
0.33 |
0.37 |
0.74 |
0.79 |
0.53 |
0.47 |
0.81 |
0.81 |
0 |
0.06 |
0.23 |
0.19 |
|
Z Angle |
0.71 |
0.61 |
0.73 |
0.18 |
0.74 |
0.44 |
0.34 |
0.01* |
0.68 |
0.06 |
0 |
0.78 |
0.90 |
|
ULPA |
0.73 |
0.51 |
0.21 |
0.45 |
0.18 |
0.24 |
0.40 |
0.55 |
0.03* |
0.23 |
0.78 |
0 |
0.01* |
|
LLPA |
0.38 |
0.85 |
0.62 |
0.85 |
0.38 |
0.93 |
0.49 |
0.20 |
0.09 |
0.19 |
0.90 |
0.01* |
0 |
When lip strain, lip morphology and interlabial gap parameters were correlated using pearson correlation in Group II, it was found that there were positive correlation of the UL-E line with LL-E(p=0.01*), LL-E with UL-B (p=0.00*),ULPA (p=0.03*), UL-S with LL-S (p=0.00*), LS with UL-S (0.02*), LL-S with LL-B (p=0.00*),LL-H (p= 0.00*) , Z-angle with ILA (p=0.02*), LL-S (0.00*), LL-H with LL-S (0.00*), ULPA with LL-E (0.03*) as depicted in [Table 9].
|
Parameters |
LS-LI |
UL-E |
LL-E |
UL-S |
LL-S |
UL-B |
LL-B |
LL-H |
NL A |
ILA |
Z Angle |
ULP A |
LLP A |
|
LS-LI |
0 |
0.70 |
0.72 |
0.74 |
0.86 |
0.63 |
0.53 |
0.36 |
0.14 |
0.28 |
0.71 |
0.73 |
0.33 |
|
UL-E |
0.70 |
0 |
0.01* |
0.96 |
0.28 |
0.92 |
0.98 |
0.38 |
0.92 |
0.96 |
0.82 |
0.12 |
0.85 |
|
LL-E |
0.68 |
0.01* |
0 |
0.27 |
0.49 |
0.00* |
0.91 |
0.34 |
0.91 |
0.38 |
0.34 |
0.03* |
0.36 |
|
UL-S |
0.77 |
0.96 |
0.98 |
0 |
0.00* |
0.00* |
0.77 |
0.14 |
0.11 |
0.66 |
0.66 |
0.15 |
0.36 |
|
LL-S |
0.85 |
0.16 |
0.98 |
0.00* |
0 |
0.70 |
0.00* |
0.00* |
0.82 |
0.51 |
0.00* |
0.59 |
0.36 |
|
UL-B |
0.70 |
0.90 |
0.03* |
0.00** |
0.00** |
0 |
0.00* |
0.11 |
0.22 |
0.99 |
0.20 |
0.01* |
0.44 |
|
LL-B |
0.55 |
0.98 |
0.19 |
0.77 |
0.19 |
0.00* * |
0 |
0.00* |
0.85 |
0.67 |
0.00* |
0.25 |
0.42 |
|
LL-H |
0.25 |
0.94 |
0.68 |
0.14 |
0.00** |
0.11 |
0.00* |
0 |
0.67 |
0.89 |
0.00* |
0.85 |
0.58 |
|
NLA |
0.18 |
0.92 |
0.91 |
0.71 |
0.82 |
0.26 |
0.85 |
0.67 |
0 |
0.65 |
0.81 |
0.11 |
0.92 |
|
ILA |
0.53 |
0.96 |
036 |
0.66 |
0.51 |
0.99 |
0.67 |
0.49 |
0.65 |
0 |
0.80 |
0.25 |
0.25 |
|
Z Angle |
0.08 |
0.82 |
0.34 |
0.67 |
0.00** |
0.20 |
0.00* |
0.00* * |
0.81 |
0.80 |
0 |
0.68 |
0.13 |
|
ULPA |
0.94 |
0.12 |
0.03* |
0.15 |
0.59 |
0.01* |
0.25 |
0.98 |
0.11 |
0.25 |
0.67 |
0 |
0.79 |
|
LLPA |
0.36 |
0.06 |
0.04* |
0.43 |
0.39 |
0.44 |
0.42 |
0.58 |
0.92 |
0.72 |
0.13 |
0.79 |
0 |
Discussion
Three crucial areas—the chin, lip, and nose—determine the profile aesthetics that are the focus of orthodontic and orthognathic treatment. Different methods can be used to evaluate soft tissue morphology, which is an essential tool in clinical practice and in research. The most appropriate and frequently used method is radiography, which offers landmarks and locations for measurements as well as a thorough evaluation of the subject's distinctive craniofacial features (Ricketts, 1981).[4] Numerous studies on the factors affecting attractive or desirable lip morphology that have focused on areas other than the profile have been conducted since lip morphology is one of the most crucial components of face aesthetics. A normal vertical-lips relationship (interlabial gap) should have a mean gap of 2 mm with the mandible in centric occlusion in normal occlusion or at the conclusion of therapy. Consequently, a minor degree of lip incompetence is common. Lip lengths, face patterns, and tooth locations are some of the elements most associated with lip incompetence. Holdaway emphasized the significance of quantifying soft tissue characteristics in orthodontic therapy and uses the distinction between the upper lip's basic thickness and its upper lip thickness for assessing upper lip strain. In cephalometric analysis, several reference lines, including the Ricketts' "E" line, Steiner's "S" line, Holdaway's "H" line, and Burstone's "B" line, are used by orthodontists in diagnosis and treatment planning to analyse the location of the upper and lower lips. [1]
Several angles have been used to evaluate facial aesthetics such as Z angle, nasolabial angle, and inferior labial angle. Burstone was one of the first workers who developed a method of direct integument analysis and applied Analysis of both dental and skeletal patterns alone may prove inadequate or misleading, for marked variation exists in the thickness, length, and postural tone of soft tissue covering the dentoskeletal framework. Graber and Vanarsdall, 2000 evaluate morphology of the upper lip in both the vertical and anteroposterior directions by measurement of the height and thickness of the upper lip, respectively. The definition of esthetics changes from one society to another, so it is important to know what esthetically fair or attractive faces are. Steiner, Ricketts, Downs, Tweed, Coben, Morgolis, Mc Namara, Sassouni and Ann Arbor have developed several cephalometric analyses and created an opinion that the normal values for one group should not be considered normal for another group. [6] The main purpose of our study was to corelate lip morphology, lip strain and inter labial gap in various skeletal malocclusions in Distt solan population.
In the present study lateral cephalograms of 50 patients who underwent orthodontic treatment were included. They were divided into 2 groups i:e Group I (skeletal Class I,N=25) and group II (Skeletal Class II,N=25) on the basis of ANB angle. Various linear and angular parameters were evaluated,compared and correlated for both the groups. When the means of various parameters were compared between skeletal Class I and Class II significant changes were seen in interlabial gap with increased value in skeletal Class II malocclusion this is because of interlabial gap increases with increase in overjet and subjects with incompetent lips were characterized by bimaxillary dentoalveolar proclination, protrusion of upper incisors, and a decreased inter-incisal angle., whereas all other parameters were found to be non-significant. This could be due to overjet relapse in the Class II malocclusion group that could be accounted for some intergroup difference. However, because there were no intergroup differences in interlabial gap behavior with time, this indirectly suggests that there were no significant relapses in over jet in the Class II group. Therefore, the initial occlusal factors of the different malocclusions no longer have an effect. In a Study done by Patrícia Bittencourt Dutra dos Santos, Daniela Gamba Garib(2013) showed similar findings which were in accordance with our study. [7] Munirah Ab Talib, Noor Shaheera Abdul Aziz, Mohammad Khursheed Alam conducted a study to evaluate the morphology of Malaysian Malay population which was in accordance with our study.[1] Avinash Chaudhary, Jamal Girimong (2022) studied the upper lip morphology which was not in concordance with our study this is due to differences in soft tissue thickness at labiomental, labrale superius, subnasal and pogonion points in Indian population. [8]
When lip strain, lip morphology and interlabial gap parameters were correlated using pearson correlation in Group I, it was found that there was positive correlation of the Upper Lip to E line with lower lip to E line this is because of protruded maxillary incisors in cases of bimaxillary protusion or patient with retroclined mandibular incisors. Measurements of the lips relative to Ricketts E-line focuses on the soft tissue balance between lips and profile (nose-chin) Almas Rahoojo, Samreen Naz (2022).[9] This result was supported by Aziz et al (2013) who reported that the upper lip of Malaysian Chinese was protrusive, but the lower lip was retrusive in relation to E line.[1] A positive correlation was seen between the Upper lip to E line with upper and lower lip to S line and with upper lip and Lower lip to B line that was due to the inclinations of upper and lower incisors which were enhanced in selected subjects presenting with bimaxillary proclination and patients with increased overjet. This was supported by the study done by Abida Ijaz, Amna Sheikh (2021) in which the study was based on the effect of lip morphology in the study sample presenting with bimaxillary dentoalveolar protrusion on normal skeletal pattern.[5] A positive relation was seen between upper Lip to S line with Lower Lip to S line because protrusive position of the Upper lip with respect to the S line and retruded lower lip in patients with convex profile with reference to S line. This study was supported by Niam R Al–Saleem (2011) on comparison of lip analyses in Skeletal Class I normal occlusion.[10] A positive correlation was seen between Upper Lip to B line with Lower Lip to B line due to the variation in lip position because of increased proclinations and overjet. Similar result can be seen in the study done by Merina Joshi, Li Peng Wu (2015) using B line in skeletal Class I & Class II group.[11] A positive correlation is seen between Upper lip protusion angle with lower lip protusion angle. Soft tissue profile also depends on the sagittal skeletal relation of the maxilla to the mandible, as the soft tissue tries to mask the skeletal discrepancies, and there is a difference in their thickness and angular measurement.
It was discovered that there was a positive association between the upper lip and lower lip to the E line in Group II when lip strain, lip morphology, and interlabial gap parameters were connected using pearson correlation. This is because Class II individuals have a protruded maxilla and a retruded mandible. The upper lip of Malaysian Chinese people was protrusive in relation to the E-line, but the lower lip was retrusive, according to a study by Khan, Fahad, and Mahroof, Verda (2017). This suggests that Asians have protruding upper lips, which may be caused by either a thick upper lip or protruding upper teeth. A positive relation was also seen between the Lower Lip to E line with Upper Lip to Burstone line and Upper Lip Angle this is concluded that the upper lip to B line was protrusive and lower lip to B line was retrusive in Skeletal class II group. In a study done by Merina Joshi, Li Peng Wu (2015) E line showed greatest variation in both Upper Lip and Lower Lip in skeletal Class I, Class II, and Class III groups, they were more protruded in Class II group. They also concluded that the upper lip to B line was protrusive and lower lip to B line was retrusive in Skeletal class II group. [11], [12] A positive relation was seen between Upper Lip to S line with Lower Lip to S line this is because protrusive position of the Upper lip with respect to the S line and retruded lower lip in patients with retrognathic profile with reference to S-line. Similar findings were observed in the study done by Bokhari, F.; Amin, F.; Asad, S (2013) on Cephalometric assessment of lips in Skeletal Class II patients by Steiner's line, Upper lip prominence was found to be statistically significantly correlated with lower incisor inclination and lower lip prominence, this may be due to Antero-posterior position of upper and lower lip in patients with retrognathic profile with reference to S-line.[13] A positive corelation was seen between lower lip to B line with upper lip to B line , Upper Lip were more protrusive and Lower Lip were retrusive in Skeletal Class II this shows the variation in upper and lower lip . Similar result can be seen in the study done by Merina Joshi, Li Peng Wu (2015) in which when using B line in skeletal class II group, Upper Lip were more protrusive and Lower Lip were retrusive in Skeletal Class II. S line and B line be the best reference lines in terms of judging the sagittal lip position in skeletal classes 11. The possible cause for the S line and the B line to be the most consistent lines may be the fact that these lines do not transverse any anatomical landmarks of the nose and the lines are close to skeletal structure. There was a negative correlation interlabial gap with all the parameters in Skeletal Class II group this is because of interlabial gap increases with increase in overjet. This result is consistent with a study by Ali H. Hassan and Azza A. Turkistani from 2014, which found that participants with incompetent lips had bimaxillary dentoalveolar proclination, protruding upper incisors, and a reduced inter-incisal angle. [14] The relationship between the Nasolabial Angle, Lower Lip protusion Angle, and Upper Lip protusion Angle was positive. [15] As the soft tissue attempts to conceal the skeletal discrepancies, there is a variation in their thickness and angular measurement, which in turn depends on the sagittal skeletal relationship of the maxilla to the mandible.
Conclusion
Upper lip thickness and the interlabial gap were observed to be significantly enlarged in cases of Skeletal Class II malocclusion based on the findings of the study stated above. Significant changes in lip morphology were observed in Skeletal Class I with increased overjet and increased proclination, while in Skeletal Class II group, values rose due to prognathic maxilla or protruded upper incisors and retrognathic mandible or retruded mandibular incisors.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Source of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- NS Abdul Aziz, MA Talib, MK Alam, R Basri, K Purmal, SA Rahman. Linear and Angular Cephalometric Lip Morphology in Malaysian Chinese Population. Int Med J 2014. [Google Scholar]
- S Anicÿ-Miloševicÿ, M Lapter-Varga, M Šlaj. Analysis of the soft tissue facial profile by means of angular measurements. Eur J Orthodon 2008. [Google Scholar]
- F Khan, V Mahroof, AK Kamran, Shafiqullah, MK Alam, I Qamruddin. Cephalometric Lip Morphology in a Sample from Pakistani Population. Int Med J 1994. [Google Scholar]
- G Abdulal, A Osman, A Abyad. Evaluation of Facial Soft-Tissue Morphology among Different Vertical Skeletal Profile. Eur Scientific J 2022. [Google Scholar] [Crossref]
- A Ijaz, A Sheikh, JI Ahmed Khan. Lip morphology a factor leading to bimaxillary dentoalveolar protrusion. Pak Oral Dent J 2011. [Google Scholar]
- M B Atit, SV Deshmukh, J Rahalkar, V Subramanian, C Naik, M Darda. Mean values of Steiner, Tweed, Ricketts and McNamara analysis in Maratha ethnic population: A cephalometric study. APOS Trends Orthod 2013. [Google Scholar] [Crossref]
- G Janson, PBD dos Santos, DG Garib, MF Francisconi, TO Baldo, SE Barros. Interlabial gap behavior with time. J World Federation Orthod 2013. [Google Scholar] [Crossref]
- A Chaudhary, J Giri, R Gyawali, PR Pokharel. A Retrospective Study Comparing Nose, Lip, and Chin Morphology in Class I, Class II, and Class III Skeletal Relationships in Patients Visiting to the Department of Orthodontics, BPKIHS: A Cephalometric Study. Int J Dent 2022. [Google Scholar] [Crossref]
- Almas Rahoojo, Samreen Naz. Soft Tissue Lip Profile with Steiner(S) and Ricketts (E) Lip Analysis in Patient’s with Skeletal and Dental Class I Occlusion. Pak J Med Health Sci 2022. [Google Scholar]
- NAl-Saleem. Comparison of Lip Analyses in Skeletal Class I Normal Occlusion and Class II Division 1 Malocclusion. Al-Rafidain Dent J 2013. [Google Scholar]
- M Joshi, L P Wu, S Maharjan, MR Regmi. Sagittal lip positions in different skeletal malocclusions: a cephalometric analysis. Prog Orthod 2015. [Google Scholar] [Crossref]
- Fahad & Khan, Mahroof, A Verda & Kamran, Shafiqullah, Alam, Irfan Mohammad & Qamruddin. Cephalometric Lip Morphology in a Sample from Pakistani Population. Int Med J 1994. [Google Scholar]
- F Bokhari, S Asad, F Amin. Cephalometric assessment of lips in skeletal class ii patients by steiner's line. 2013. [Google Scholar]
- AH Hassan, AA Turkistani, MH Hassan. Skeletal and dental characteristics of subjects with incompetent lips. Saudi Med J 2014. [Google Scholar]
- E Sarilita, C Rynn, P A Mossey, S Black, F Oscandar. Facial average soft tissue depth variation based on skeletal classes in Indonesian adult population: A retrospective lateral cephalometric study. Leg. Med 2020. [Google Scholar] [Crossref]
