- Visibility 14 Views
- Downloads 3 Downloads
- DOI 10.18231/j.jdp.2023.027
-
CrossMark
- Citation
Unraveling telangiectatic granuloma: A case report of an enigmatic oral lesion in the posterior mandibular region
Introduction
Telangiectatic granuloma is a relatively rare oral lesion characterized by a proliferation of small blood vessels and granulation tissue. Its occurrence in the oral cavity is often associated with local irritants, trauma, or chronic inflammation. Smokeless tobacco use has been implicated as a risk factor for the development of various oral lesions, including telangiectatic granulomas. This case report describes the diagnosis and management of a telangiectatic granuloma in a patient with a history of smokeless tobacco consumption.
Case Presentation
A 45-year-old male patient presented with a complaint of swelling in the lower right back posterior region of the jaw, accompanied by pain and difficulty in swallowing. The patient had noticed a small growth 2-3 months prior, which had rapidly increased in size over the past 15-20 days. The patient's medical history included jaundice five to six years ago, while his dental history revealed that this was his first dental visit. The patient reported a long-term consumption of smokeless tobacco, combining areca nut, betel leaf, and tobacco in quid form. Oral hygiene habits were suboptimal, with infrequent tooth brushing and evidence of tobacco stains on the teeth.
Clinical Examination
The patient's vital signs were within normal limits. Hard tissue examination revealed disto-proximal caries in tooth 33 and traumatic occlusion. Attrition and gingival recession were noted in several teeth. The gingiva appeared enlarged, soft, and edematous, with a reddish-pink color. Linear marginal gingival erythema and stains with calculus were also observed.

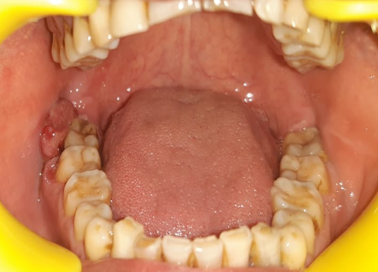
A grayish-white plaque was evident on the lower anterior vestibule extending from the distal surface of the left canine to the right canine region. The plaque appeared as a separate entity from the proliferative pedunculated growth on the lower right buccal mucosa.

A proliferative pedunculated growth was observed on the lower right buccal mucosa, measuring approximately 20x30 mm in size. The lesion had irregular borders, an ovoid shape, and a reddish-pink color. The surrounding mucosa appeared normal. The lesion was painless, had a soft and friable consistency, and was non-tender. Profuse bleeding was associated with trauma from tooth brushing or mastication. The outer part of the lesion appeared reddish-pink, while the inner part was white reddish. Based on the clinical presentation, the provisional diagnosis of pyogenic granuloma was made for the proliferative pedunculated growth (48).

Other findings noted
Tobacco pouch keratosis was observed in the lower vestibule, affecting the lower right and left anterior regions (43, 42, 41, 31, 32). The patient also presented with chronic generalized marginal gingivitis and localized periodontitis in the lower mandibular anterior region (43, 42, 41, 31, 32). Chronic reversible pulpitis was diagnosed in tooth 33.
Based on these findings an orthopantomogram was advised that showed the following features.
An orthopantomogram (OPG) revealed disto-proximal caries in tooth 33, generalized bone loss, and radiolucency in the inferior cortex of the mandible with tooth 33. The shape of the condyles appeared round on the right side and flat on the left side, with decreased space in between the glenoidal fossa seen on the left condyle.

Histopathological analysis
An excisional biopsy was performed on a pedunculated growth located on the lower right buccal mucosa, specifically around tooth 48. The excised specimen was preserved in 10% formalin and sent for histopathological analysis. The examination revealed parakeratinized stratified squamous epithelium and the underlying connective tissue. The epithelium exhibited ulceration in certain areas. The connective tissue displayed collagen fibers interspersed with fibroblasts and abundant blood vessels. The vessels varied in size, some of which were engorged with red blood cells and showed endothelial cell proliferation. A chronic inflammatory infiltrate consisting of lymphocytes and plasma cells was also observed. The histopathological examination confirmed the diagnosis of telangiectatic granuloma.

Based on clinico -pathologic correlation, the lesion was diagnosed as Telangiectatic Granuloma.
The treatment plan was devised as follows:
In the emergency phase, an excisional biopsy (48) was recommended for histopathological analysis to obtain a definitive diagnosis. In Phase I the patient was educated about the harmful effects of smokeless tobacco and advised to gradually quit the habit. A follow-up appointment was scheduled after one month. Additionally, oral hygiene instructions were provided, and oral prophylaxis was advised.
Phase II involved surgical/periodontal procedures such as scaling and root planning to address the chronic generalized marginal gingivitis and localized periodontitis in the lower mandibular anterior region (teeth 43, 42, 41, 31, 32). If necessary, root canal treatment may be performed for tooth 33, which is experiencing chronic reversible pulpitis.
Phase III focused on restorative treatment, including addressing the disto-proximal caries in tooth 33 and considering extraction if needed for tooth 48, based on the findings of the histopathologic evaluation and assessment of the dilaceration and possible peripheral giant cell granuloma/ossifying fibroma.
In Phase IV, a rehabilitation phase, an occlusal splint was recommended to manage the patient's history of bruxism (nighttime teeth grinding) and address any issues related to traumatic occlusion, if deemed necessary after a comprehensive evaluation.
Phase V is the maintenance phase, which involves regular recall appointments, including one scheduled after one week to monitor the healing and progress of the excisional biopsy site (exophytic lesion). Another follow-up visit after one month will assess the patient's progress in quitting smokeless tobacco. Long-term maintenance visits will be scheduled to monitor oral health, provide necessary treatments such as oral prophylaxis, and reinforce proper oral hygiene practices.
Unfortunately, the patient did not return for the scheduled follow-up appointment as advised in the treatment plan.
In the case of telangiectatic granuloma, platelet rich fibrin (PRF) can promote the healing process and help in the management of the condition. When PRF is applied to the affected area, the growth factors present in the fibrin matrix stimulate tissue regeneration, angiogenesis, and the production of collagen. This can aid in reducing the dilated blood vessels, controlling fibrous tissue proliferation, and modulating the chronic inflammatory response associated with telangiectatic granuloma.
Discussion
A pyogenic granuloma or lobular capillary hemangioma [1] is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. [2], [3] It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh. [4] This disease was first recognized by Poncet and Dor in 1897 as a “botryomycosis hominis”. It has since been known by a variety of names including lobular capillary hemangioma, granuloma pyogenicum, and granuloma telangiectaticum.
Telangiectatic granuloma is popularly also referred to as pyogenic granuloma, it’s a benign, hyperplastic, inflammatory, fast growing lesion of the soft tissues that easily bleeds, [5] on provocation and may be dermatological or oral origin affecting the skin, oral mucosa, gingiva, lips, tongue. It is a common reactive neoformation[6] that develops as a response to varied stimuli such as hormonal factors, local trauma and certain drugs or chronic irritation creating a repair tissue (granulation) produced by the body as a defense mechanism. [7] The name "hemangiomatous granuloma," which expresses histopathologically like hemangioma and the inflammatory nature (granuloma) of oral pyogenic granuloma, was proposed by Angelopoulos AP. [8]
Due to the existence of different blood arteries in oral pyogenic granulomas, Cawson et al proposed the term "Granuloma Telangiectacticum." [9] Pyogenic granulomas may be seen at any age, and are more common in females than males.
Several factors have been implicated in the development of telangiectatic granuloma, including poor oral hygiene, ill-fitting oral appliances, overhang margins of dental restorations, and persistent bite trauma. The management of oral telangiectatic granuloma involves maintaining good oral hygiene, curettage of the lesion base, surgical excision to decrease the frequency of recurrence, accompanied by antibiotic and analgesic therapy.
Clinically, telangiectatic granuloma presents as a pedunculated, easily bleeding tumor, often located in the anterior maxillary gingiva. Clinical correlation should be performed for the different phases of pyogenic granuloma, with younger lesions being red to purple due to strong vascularity and later lesions becoming collagenized and appearing pink.[10] Proper histopathological examination is crucial for an accurate diagnosis and to differentiate it from other oral lesions with similar clinical features.
The treatment of choice for telangiectatic granuloma is excisional surgery involving the periosteum. Complete removal of the lesion is essential to minimize the risk of recurrence. Alternative treatment modalities, such as cryosurgery, laser excision, and sclerotherapy, have also been reported with varying success rates. However, despite these treatments, recurrence is not uncommon, and re-excision may be required in some cases.
Conclusions
Telangiectatic granuloma is a reactive vascular soft tissue proliferation commonly found in the oral cavity. It is associated with chronic irritation, poor oral hygiene, and trauma. Accurate diagnosis and appropriate management are crucial to prevent misdiagnosis and ensure complete removal of the lesion. Long-term follow-up and patient education regarding oral hygiene practices and the avoidance of chronic irritants, such as tobacco, are essential to prevent recurrence and promote oral health. Further research is warranted to better understand the pathogenesis and optimal management of telangiectatic granuloma.
Source of Funding
None.
Conflict of Interest
There is no conflict of interest
References
- N Pernick. "Oral cavity & oropharynx - Other nonneoplastic - Pyogenic granuloma". PathologyOutlines. Topic Completed: 1 November 2013. Minor changes: 12 October 2020. . [Google Scholar]
- IM Freedberg, AZ Eisen, K Wolff, KF Austen, LA Goldsmith, SI Katz. . Fitzpatrick's Dermatology in General Medicine 2003. [Google Scholar]
- H Jafarzadeh, M Sanatkhani, N Mohtasham, Nooshin Mohtasham. Oral pyogenic granuloma: a review. J Oral Sci 2006. [Google Scholar] [Crossref]
- Peter M Nthumba. Giant pyogenic granuloma of the thigh: a case report. J Med Case Rep 2008. [Google Scholar] [Crossref]
- JH Ricardo, A López, K Romero. Oral telangiectatic granuloma. Case series presentation. Rev Fac Odontol Univ Antioq 2012. [Google Scholar]
- K Patil, V G Mahima, K Lahari. Extragingival pyogenic granuloma. Indian J Dent Res 2006. [Google Scholar]
- P Ghodke, R Hegde, S Lambe, W Ansari, S Muglikar. Management of Oral Telangiectatic Granuloma with 810 nm Diode Laser in a Medically Compromised Patient: A Case Report. Dentist 2019. [Google Scholar]
- AP Angelopoulos. Pyogenic granuloma of the oral cavity: Statistical analysis of its clinical features. J Oral Surg 1971. [Google Scholar]
- RA Cawson, WH Binnie, PM Speight, AW Barrett, JM Wright. . Lucas Pathology of tumors of oral tissues 1998. [Google Scholar]
- SR Gomes, QJ Shakir, PV Thaker, JK Tavadia. Pyogenic granuloma of the gingiva: a misnomer?-a case report and review of literature. J Indian Soc Periodontol 2013. [Google Scholar]
