- Visibility 83 Views
- Downloads 17 Downloads
- DOI 10.18231/j.jdp.2023.028
-
CrossMark
- Citation
Unilateral gingival enlargement in a patient with neurofibromatosis type 1 - Case report
- Author Details:
-
Sherin Ann Thomas *
-
Aashmi Pradeeba Das T H
-
Asish Rajasekharan
-
Girija K L
-
Soumya Gopinadh
Introduction
Neurofibromatosis (NF) is a group of autosomal dominant genetic disorders, first described by Friedrich Daniel Recklinghausen in 1882. It is characterized by multiple cutaneous lesions and tumors in the central and peripheral nervous system. [1] NF is divided into two distinct types, NF type 1 (NF-1) and NF type 2 (NF-2). NF-1 was. NF-1 is an autosomal dominant genetic disease that affects 1 in 3000 newborns; [2] Mutations with no family history of NF contribute to about 50% of cases. It usually occurs in the 3rd decade of life, without any sexual predilection. Clinically, neurofibroma is a slow-growing pedunculated or sessile nodule. It is usually painless, but pain and paresthesia may occur due to nerve compression. Although the tongue is the most common site of intraoral involvement, it can also be found in other regions such as the palate, buccal mucosa, floor of the mouth, and mandible. [3] Hyperpigmentation of the skin (called cafe-au-lait spots) and spots in the axillary or inguinal (crowe’s sign) are characteristic signs of the disease. Lisch nodules in the iris are seen in almost all patients. Gingival enlargement is a common finding in NF-1 patients. These swellings are widespread, non-tender and fibrous, and there is no sign of inflammation. Here we present a case of neurofibromatosis type I with unilateral painless gingival enlargement.
Case Report
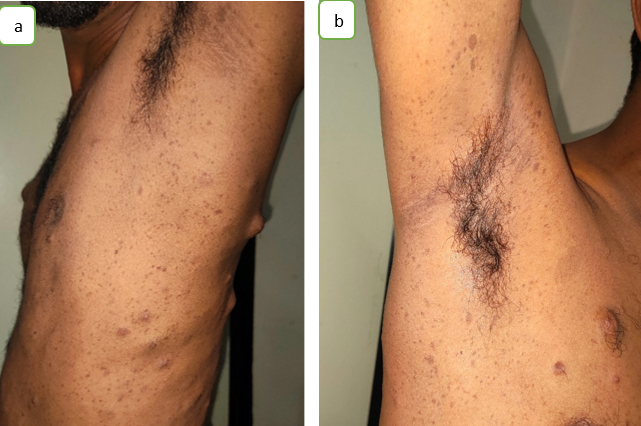
A 26-year-old male patient reported to the Department of Oral Medicine and Radiology with a chief complaint of pain in the left lower tooth region for 4 days. On intraoral examination, gingival enlargement was observed on the buccal and lingual aspects of the mandibular teeth, with involvement of marginal and interdental papillae extending from 43 to 38 region. The swelling was smooth, normal in color and surface. On palpation, the buccal aspect of the lesion was nontender and firm, and the lingual aspect was soft. Displacement of teeth with spacing noted between 31,32,41,42. Hard tissue examination revealed deep dentinal caries in 46 and tender, inflamed tissue around partially erupted 38. In general and extraoral examination; multiple cutaneous nodules of various sizes were seen throughout the body, including the face, neck, upper and lower extremities, chest, and back. Brown-colored hyperpigmented patches (Cafe – au – lait pigmentation) noted on neck, chest and back. Multiple Lisch nodules were seen in the iris. Axillary freckling was also noted on both sides. Family history revealed that his father has similar lesions all over the body and face. After further analysis, panoramic radiographs showed deep dentin caries with pulp involvement and periapical abscess in 36,37. Periodontal ligament widening with loss of lamina dura was noted in 26,27,28,31,32,33,34,35,36,37,38.41,42,43,44,45,46,47,48. Mild to moderate bone loss was noted in both maxillary and mandibular teeth. Irregular widening of the left lnferior alveolar nerve canal was also noted.

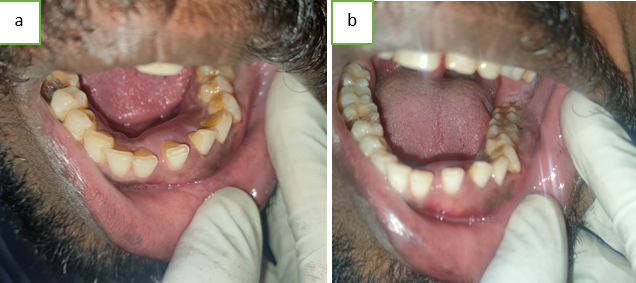

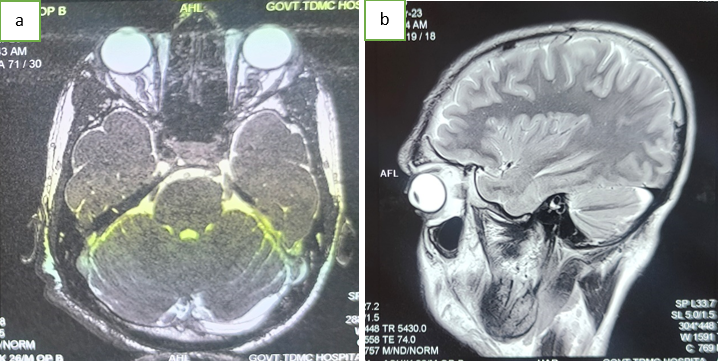
Based on the clinical examination and radiographic findings a provisional diagnosis of Gingival enlargement secondary to neurofibromatosis was made and the patient was referred to the department of Dermatology and venereology for expert opinion. He was diagnosed with Neurofibromatosis type -1 in the department of dermatology and was send for further neurologic, ophthalmic, cardiology, ENT and orthopedic consultation to look for CNS involvement, presence of lisch nodules, optic glioma, rhabdomyoma, bony deformities, and acoustic neuromas. His MRI report revealed multiple hyperintense areas in bilateral basal ganglia, right cerebellar hemisphere and brainstem. Left optic nerve appeared thickened and fusiform in shape and appeared to be optic glioma. A hyperintense extracalvarial lesion was noted in the right frontotemporoparietal concavity suggestive of plexiform neurofibroma. Initially, the patient was managed with nonsurgical periodontal therapy including scaling, root planning and restoration of 46. Comprehensive periodontal flap surgery for the periodontally involved teeth was performed and the patient was planned to be kept under periodic follow-up.
Discussion
The diagnosis of NF1 and NF2 is based on clinical criteria. The diagnostic criteria include the appearance of two or more of the following: cafe-au-lait spots, two or more neurofibromas, freckling in the axillary and inguinal regions, optic pathway tumour, lisch nodules and distinctive osseous lesions. [4] Pigmented lesion is one of the most common manifestations, can often appear at birth or in the first year of life. The pigmented lesions appear as cafe-au-lait spots and freckles.[5] This patient reported multiple cafe-au-lait spots and axillary freckling’s which appeared during childhood and showed multiple lisch nodules in the iris. Neurofibromas are benign complex tumours arising from peripheral nerve sheaths, which constitute one of the main manifestations of NF1. Clinically they appear as either discrete or localized and plexiform neurofibromas.[6] Neurofibromas, although most commonly seen on skin, but can involve many organs including stomach, intestines, kidney, bladder, larynx and heart. This patient revealed multiple plexiform lesions in the face, neck, upper and lower limbs, chest and back region. Osseous alterations may be seen in more than half of the patients with neurofibromatosis. Radiographic findings of the lesions involving the mandible include enlargement of the mandibular foramen (34%), enlargement of mandibular canal (29%), or branching of the mandibular canal (24%).[3], [7] This patient showed irregular widening of left inferior alveolar nerve canal and mental foramen in the panoramic radiograph. Among the oral mucosal sites tongue and buccal mucosa are the most common sites. Diffuse macroglossia can also be present. Among main clinical manifestations of the disease are high prevalence of increased prominence of fungiform papillae, which occurs in 50% of the cases and it is the most frequent finding. Our patient also showed prominent fungiform papillae in the tongue. Shapiro et al stated that the involvement of the gingiva is 5%. [3], [8] In this case enlargement of the gingiva noted in the buccal and lingual aspect of mandibular teeth, extending from 43 to 38 region. NF1 commonly leads to tongue and gingival tissue overgrowth, which can progress to oral cancer. Hence, regular monitoring is essential to detect the occurrence of overgrowth in these patients.
Conclusion
Recognition of oral manifestations in patients with NF-1 is important since in many cases dentist may be the first one to notice these changes before the diagnosis. It is known that nodules are recurrent and the patient has increased tendency to develop optic gliomas, malignant peripheral nerve sheath tumor, vascular malformations, aneurysms, stroke etc it is crucial to keep patients under observation, carrying out a long-term follow-up in order to track new changes and treat them accordingly.
Source of Funding
None.
Conflict of Interest
There is no conflict of interest
References
- P Ghalayani, Z Saberi, F Sardari. Neurofibromatosis type I (von Recklinghausen’s disease): A family case report and literature review. Dent Res J (Isfahan) 2012. [Google Scholar]
- S Prud’homme T, Dajean-Trutaud, Z Badran, Hyon I Wotjiuk, F. Dental Management of Neurofibromatosis Type 1: A Case Report and Literature Review. Int J Clin Pediatr Dent 2019. [Google Scholar] [Crossref]
- SD Shapiro, K Abramovitch, ML Van Dis, LJ Skoczylas, RP Langlais, RJ Jorgenson. Neurofibromatosis: oral and radiographic manifestations. Oral Surg Oral Med Oral Pathol 1984. [Google Scholar] [Crossref]
- V Shekar, V Rangdhol, J W Baliah, S Thirunavukarasu. An unusual oral manifestation of type 1 neurofibromatosis: A case report and review of literature. J Nat Sci Biol Med 2015. [Google Scholar]
- O Bekisz, F Darimont, E H Rompen. Diffuse but unilateral gingival enlargement associated with von Recklinghausen neurofibromatosis: a case report. J Clin Periodontol 2000. [Google Scholar]
- H Cherifi, B Fournier, A Berdal, B Mcalpin, IY Sitbon, B Gogly. Oral Manifestations of Neurofibromatosis Type 1. J Cosmet Dermatological Sci Appl 2019. [Google Scholar]
- MT Fadda, G Verdino, MC Mustazza, D Bartoli, G Iannetti. Intra-parotid facial nerve multiple plexiform neurofibroma in patient with NF1. Int J Pediatr Otorhinolaryngol 2008. [Google Scholar]
- B Shetty, Y Umesh, K Kranti, H Seshan. Periodontal manifestations of von Recklinghausen neuro fibromatosis. J Indian Soc Periodontol 2013. [Google Scholar]
How to Cite This Article
Vancouver
Thomas SA, H APDT, Rajasekharan A, L GK, Gopinadh S. Unilateral gingival enlargement in a patient with neurofibromatosis type 1 - Case report [Internet]. J Dent Panacea. 2025 [cited 2025 Sep 07];5(3):126-129. Available from: https://doi.org/10.18231/j.jdp.2023.028
APA
Thomas, S. A., H, A. P. D. T., Rajasekharan, A., L, G. K., Gopinadh, S. (2025). Unilateral gingival enlargement in a patient with neurofibromatosis type 1 - Case report. J Dent Panacea, 5(3), 126-129. https://doi.org/10.18231/j.jdp.2023.028
MLA
Thomas, Sherin Ann, H, Aashmi Pradeeba Das T, Rajasekharan, Asish, L, Girija K, Gopinadh, Soumya. "Unilateral gingival enlargement in a patient with neurofibromatosis type 1 - Case report." J Dent Panacea, vol. 5, no. 3, 2025, pp. 126-129. https://doi.org/10.18231/j.jdp.2023.028
Chicago
Thomas, S. A., H, A. P. D. T., Rajasekharan, A., L, G. K., Gopinadh, S.. "Unilateral gingival enlargement in a patient with neurofibromatosis type 1 - Case report." J Dent Panacea 5, no. 3 (2025): 126-129. https://doi.org/10.18231/j.jdp.2023.028
