Introduction
Due to the inherent variation of intra-cranial Cephalometric Reference Structures, an assessment based on them may be inaccurate, which can have serious consequences for the planning of orthodontics and orthognathic surgical procedures. 1, 2 In cephalometric analysis, a head orientation that is readily applied, repeatable, and the most accurate depiction of the head orientation in real life is necessary for the application of a genuine vertical or horizontal extracranial reference plane. The head position that is recorded should also show the skull and cervical spine in their typical, biologically regular positions. To achieve such a posture, the head and neck muscles would need to be coordinated in a repeatable manner. A frequent craniofacial reference plane is the Sella-Nasion (SN) plane, which is the anterior cranial base plane.3 Since this plane represented the anterior cranial base, it was seen as dependable. Another popular reference plane is the Frankfort Horizontal Plane (FHP), which is thought to represent the most precise estimation of a True Horizontal (TH) plane.4 The TH plane differed significantly from the SN plane and FH plane, according to a literature assessment published by Madsen et al.5 The FH plane differed on average 1-5° from the TH plane, whereas the SN plane had considerable interobserver variability of 2-9°. It would thus be questionable how reliable it would be to use the SN and FH planes as reference planes. However, because the landmarks for all intracranial reference lines are not stable points in the cranium and are subject to biologic variation in the vertical relationship of their landmarks, cephalometric findings may be deceptive when using the nasion-sella line in the anterior skull base as a reference line.
Zebeib et al.6 compared TH planes with horizontal anatomic planes in their study, whereas Lundstrom et al. compared TH planes with SN planes, FH planes, and Ba-N planes. These two experiments supported the idea that, when taken correctly in Natural head position (NHP), the FH plane should be near the TH plane. In orthodontics, natural head position, or NHP, was first used in the late 1950s.4, 7, 8 Broca 9 defined this head position as “when man is standing and his visual axis is horizontal, he is in the natural position”. A typical method of registering natural head position is based on Solow and Tallgren’s10, 11 work in which subjects are asked to stand in “orthoposition” 8 and look into their own eyes in a mirror after a series of neck flexion exercises. Other methods of NHP registration include instructing subjects to look at a small light,12 the use of a fluid level device,13 an operator estimated “Natural Head Orientation (NHO)”14 and the use of an inclinometer.15
The primary reason for supporting NHP as a craniofacial reference system is its strong intra-individual repeatability to a realistic vertical plumb line on two or more times. Furthermore, NHP's easy registration and accurate depiction of a real-life look warrant its application in cephalometric analysis. 3, 16 NHP isn't used very often, though, maybe because of practical issues like staff training and equipment requirements. As a result, it has been shown that a more reliable craniofacial reference system is represented by real vertical or horizontal planes obtained from an NHP registration. Other intracranial planes tested for validity by evaluating inter-individual variability and average orientation include the palatal, functional occlusal, mandibular, Y axis, nasion-pogonion, A point-B point, 17 basion-nasion,3 and pterygomaxillary vertical. 18 All these craniofacial planes have been shown to display variability as large as FH and SN. In a 1950 study on facial prognathism, Björk 19 brought attention to the inaccuracy of intracranial reference lines. Bjork saw two people who were almost similar in profile but showed a significant variance in the inclination of their cranial bases instead of variations in prognathism. One of the earliest researchers to note the average orientation and inter-individual variability of the Frankfort Horizontal as a reference plane was Downs 20 in 1952. According to Downs, the Frankfort Horizontal mean position had an average variation of -0.9° from the real horizontal and a standard deviation of 5°. Downs 8 retested this idea in 1956 and came up with similar findings. Frankfort Horizontal had an average variation of -1.3° from true horizontal and a standard deviation of 5°. While recording a natural, free-balanced head position, the subject's tenseness and eagerness were mentioned as potential sources of inaccuracy. This head posture needed to be determined with some discretion.
The vestibular system, in conjunction with visual information and the strength of the supporting muscles, regulates head position. 21 Twenty muscles in the neck contract as the head moves side to side or in different oscillations up and down. Patients' heads are physiologically stabilised in the sagittal and axial planes by use of two reflexes. The first is the vestibulocollic reflex, in which the neck's muscles react to input from the vestibule. The second controls the neck's reaction to stretch receptors and is known as the cervico-collic reflex. When a person sits or stands in the same position, positional memory, muscular tone, muscle memory, and visual reaction work together to maintain positional stability in the sagittal plane. 22
NHP is essentially a consistent, repeatable head posture in which the individual looks straight ahead at a far-off object. These far-off objects might be the horizon, a light source at eye level, or one's reflection in a mirror. This head attitude is thought to be somewhat similar to the typical physiological one that people adopt on a regular basis.
Factors Associated with Natural Head Position
NHP is dynamic in its nature. Individuals vary their head posture and NHP depending on the physiological and environmental demands. Several factors appear to affect head posture. These include:
Craniofacial Morphology
Björk 23, 24 in 1955 and 1960 and Brodie 25 in 1971 referred to how the head position has a propensity to conceal its morphology. Bench 26 in 1963 reported that the neck was curved in brachycephalic types and relatively straight in dolichocephalic types.
Weight of head and effect of Gravity
As gravity negatively affects the head's equilibrium and alignment with the spine, it is possible that the weight of the head plays a substantial role in the result that patients exhibit more deviation in the sagittal plane while assuming NHP. 27
Walking
The majority of the research on NHP and head posture discusses standing or sitting in a static position. In real life, head posture is not static; rather, there is a spectrum of head orientations centred around a mean head orientation. Usumez and co-workers 28 in 2006, used readings from eyewear inclinometers to compare walking and static head positions. Fifty respondents' head positions were compared during a 5-minute, calm stroll and during a "self-balanced" head posture. In comparison to the mean static head position, the mean walking head position was 4.6° tilted downward.
Respiratory resistance
Early research on children who were judged to need adenoidectomy was published by Woodside and Linder-Aronson 29 in 1979. When comparing these children's head postures to normal nasal breathing controls, they discovered that they were either 6° bent backward or stretched forward from the real vertical. One month following adenoidectomy, the difference in intergroup head position was no longer noticeable. In 1984, Solow and colleagues 30 looked into this association and discovered that a higher cranio-cervical and cranio-vertical angulation was often linked to blockage or decreased nasopharyngeal airway adequacy. This is corroborated by several studies.31 Head extension has also been linked to obstructive sleep apnea.32, 33, 34 Thurow demonstrated that when the head is stretched, a passive stretch of the suprahyoid muscles pulls the hyoid bone forward. Mouth breathers frequently exhibit this kind of cranial extension, and this postural shift may serve as a significant compensatory mechanism for insufficient nasal airway capacity. 35
Rapid maxillary expansion
In 2005, Tecco and colleagues36 observed the head posture of 23 female participants following RME treatment. They discovered a statistically significant rise in the cervical lordosis angle, flexion of the head, and decrease in cranio-cervical angulation in addition to a statistically significant increase in pm-Ad 2, the narrowest portion of the nasopharyngeal airway. In a similar investigation by McGuiness & McDonald 37 in 2006, 43 subjects were followed up immediately and 1 year after RME. No change in head posture was noticed immediately after expansion. One year post expansion, however, NSL/VER had reduced by 3.14°, OPT/HOR by 2.13° and CVT/HOR by 2.55°. The authors explain this variation as the result of switching from oral to nasal breathing. The mechanism of this alteration might be connected to Solow and Kreiborg's soft tissue stretching theory. 38
Orthognathic surgery
Savjani et al. 39 in 2005 investigated the change in cranio-cervical angle after orthognathic surgery performed on thirty-three participants to alter their vertical facial height. The results revealed that while neck posture improved (NSL/OPT), head position remained same (NSL/VER). The investigators did come to the conclusion that surgery had nothing to do with this alteration in neck position.
Functional appliance
Following functional appliance therapy, the cervical spine position was evaluated by Tecco and colleagues. 40 The study compared twenty female patients receiving FR-2 regulator treatment to twenty untreated Class II controls. At the conclusion of therapy, the cervical lordosis angle (CVT/EVT) in the study group was substantially greater than in the control group. This was likely caused by a large backward inclination of the upper segment of the cervical column (OPTNer and CVTNer) in the treated group from the pre- to post-treatment period. The cervical column's inclination in the lower segment (EVT/VER) did not significantly change. Cleall 41 showed that when an intraoral appliance is inserted, the tongue is displaced, leading to cranial extension. A transpalatal bar put as part of orthodontic therapy also causes cranial extension beyond the usual cranial position. By encroaching on the oral cavity, the appliances push the tongue out of its natural position. 42
Craniomandibular disorder
Using the craniovertebral angle created by the McGregor plane to the odontoid plane, Valenzuela et al. 43 studied head posture in 2005. Based on the extent of this angle, the sample of fifty patients was split into three groups: head flexion (greater than 106 degrees), head extension (less than 95 degrees), and an arbitrary normal head posture (between 95 and 106 degrees). There was no correlation discovered between the incidence of CMD and these head position groups.
Altered vision
Fjellvang and Solow 44 studied a control group of 171 dentistry students (aged between 22 and 30 years) and 30 blind patients from birth subjects (aged between 15 and 35 years). The head postures of blind respondents varied more on average. Furthermore, the neck was inclined 4.5° farther forward than in the control group, and the head was angled 4.3° lower than in the group. In both groups, the cranio-cervical angle was comparable.
Methods of Recording Natural Head Position
Von Baer 45 published a description of one of the earliest methods for recording NHP in 1861. The patients were told to take a seat on a stool in a calm and comfortable manner. In the process, individuals were instructed to stare into a circular mirror that was positioned at the same height as their eyeballs. This initial approach has been adapted for use in the majority of subsequent research. In the historic study by Downs 8 published in 1956, the first orthodontic article pertaining to NHP was found. In order to provide a rational method of soft tissue profile typing, the goal of this work was to distinguish harmonious dentofacial profiles from inharmonious ones. Downs had 100 kids stand in front of a mirror, staring into their own eyes, and taking pictures of their lateral head profiles. To demonstrate how corrections for people whose Frankfort plane is not horizontal eliminate differences in face typing, he suggested having the individual stand and gaze at a far-off object.
In 1958, Moorrees and Kean 4 released another seminal work outlining a comparable NHP registration technique. To radiographically register the patient in NHP, they modified Von Baer's head registration technique. Before the individuals were exposed to lateral head radiographs, they were put in NHP within the cephalostat. A vertical stainless-steel wire on the radiograph cassette, which served as a real vertical reference plane, was caught on the resulting film, which showed NHP. When the individuals were seated, a mirror with a diameter of 100 mm that was affixed to the wall 170 cm distant at the level of the transmeatal axis served as a reference for head alignment.
A study comparing the self-balance head position during lateral head radiography and the mirror guided NHP was published in 1971 by Solow and Tallgren.10 The modified cephalostat, which bore a remarkable resemblance to the setup used by Moorrees and Kean, 4 held 120 individuals. Every participant was in "orthoposition",11 which was attained by having them walk on the spot. After doing head bending exercises (tilting their head back and forth with decreasing amplitude), the subjects' own sense of natural head balance was used to determine the self-balancing position film exposure. The first fluid level device was introduced by Showfety7 in 1983 to replicate a subject's NHP to the cephalostat during a lateral head film exposure. This apparatus makes use of a liquid's constant horizontal surface in a hydrostatic system that is not accelerating such that the surface is perpendicular to the force of gravity. The subject's temple was fitted with a tiny pivot bracket holding this little fluid gadget, which was fastened there using double-sided tape. After that, the fluid level is adjusted to be horizontal in accordance with the NHP. After telling the patient to step inside the cephalostat and modify their head tilt such that the fluid level is horizontal, the film is exposed.
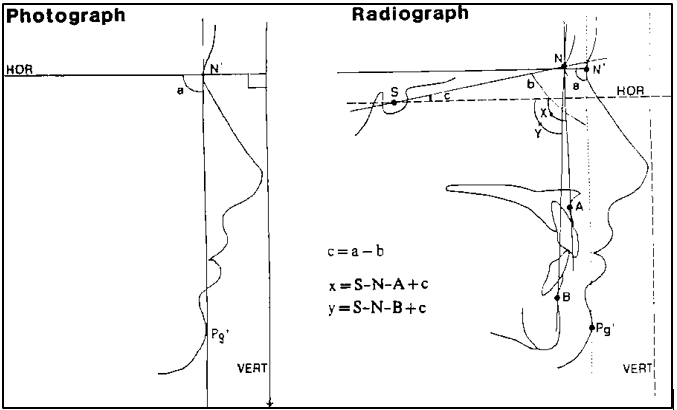
First to describe a photographic method for converting NHP to a lateral cephalometric film was Lundström and Lundström in 1992. 3 In this method, 52 participants obtained an NHP by placing their teeth in light-centric occlusion, standing in Mølhave's orthoposition, and staring at a vertical mirror that was one meter distant. To show the real vertical, a plumb line was employed, and lateral head shots were captured. From each image, a horizontal line perpendicular to the vertical plumb line was transferred to the matching lateral head radiograph. 1 The initial step in this transfer approach was to measure the angle (a) between the true horizontal reference plane, or HOR, on the picture (Figure 1) and the soft tissue nasion-pogonion (N'-Pg'). On the radiograph, a second angle (b) from SN/N'-Pg was noted. The angle (c) of SN to HOR was then calculated using simple mathematics as shown. By presenting the idea of "Natural Head Orientation (NHO)" as a technique for registering natural head position, Lundström and Lundström 3 further their research in this field. In a standing, relaxed body and head posture, NHO refers to a head orientation that the clinician, based on overall experience, perceives as the natural head position while the individual is staring at a distant point at eye level.
Advantages
It provides an extracranial reference line for cephalometric study,
The NHP of individuals is relatively constant over time with least biological changes,
Since it represents the true-life appearance of subjects, therefore it can be used for profile evaluation and direct comparison between facial appearance and cephalometric tracings.
Conclusion
Because of its accurate depiction of head orientation, simplicity of registration, and strong intra-individual repeatability when compared to the true vertical, NHP stands to be a viable alternative to traditional craniofacial reference planes. When it comes to true horizontality, NHP can be successfully replicated within 2-3°, which is less than the inter-individual variability of Sella-nasion or Frankfort Horizontal. A mirror-guided approach is the most widely recognized natural head registration procedure, and it involves standing in orthoposition and doing basic neck-bending exercises. The most clinically acceptable repeatable posture is the natural head position, and the real horizontal planes obtained by NHP registration provide a more reliable craniofacial reference system. To enhance its therapeutic uses, cephalometrics is continuously improving its methods and analysis. Notwithstanding the numerous approaches that have been put out to develop NHP, practical challenges in the therapeutic setting make it difficult for physicians to fully apply the notion of NHP throughout the course of therapy.