Introduction
Fingerprints were used on pottery thousands of years before Christ's birth to identify the creator and brand. In Egypt's tomb of King Tut-en-Khamen, slabs of clay 3,000 years old and bearing fingerprints were discovered.1 Dermatoglyphics has been implicated in a variety of medical and dental disorders, one of which is dental occlusion. Since the development of the teeth and the palate occurs at the same time as the formation of dermal patterns, there is a link between dermatoglyphics and dental occlusion. Specific Dermatoglyphic patterns were initially associated with Down's syndrome, a hereditary condition, by Cummins in 1939. Dermatoglyphics, according to Galton in 1965, is the study of dermal ridge counts and patterns on the fingers, palms, and soles. According to Adams and Niswander (1967), patients with cleft lip and palate, a disorder that is thought to have a polygenic base, exhibit developmental instability in the form of asymmetry in their dental and dermatoglyphic patterns. In 1968, Holt discovered that the inheritance of cutaneous features is thought to follow a traditional polygenic model. Dermatoglyphics' predictive validity in medical biology was bolstered by Holt (1968) and Verbov (1970), who proposed that it may help with the identification of both genetically and non-genetically determined diseases.2
Significant progress has been made in recent decades in determining the connections between dental disease and dermatoglyphic patterns. Malocclusion, a frequent dental disorder that affects facial attractiveness, involves misaligned teeth, incorrectly positioned jaws, or a combination of the two. The lip, alveolus, and palate can alter according to hereditary and environmental circumstances, and irregularities in the appearance of finger and palm prints may also result. In this way, the genetic information present in the genome at this time is reflected in the dermatoglyphic patterns. Thus, dermatoglyphics demonstrate their value as a screening tool and aid in solidifying the diagnosis. Additionally, some sagittal skeletal discrepancies might benefit from early interceptive therapy by using this method.3
In 1970, Poch and Smith discovered that dermal ridges begin to form from the 13th week of intrauterine life and stay constant throughout the rest of a person's life, serving as a mark of individuality. Whorl, loop, and arch patterns are the three different forms of dermatoglyphic patterns. Compared to Loop and Arch, Whorl has two deltas, one delta, and one central delta, respectively. Depending on the side to which the loop opens, loop patterns are further divided into Ulnar and Radial loops.4 The two sorts of ridges that are created are primary and secondary ridges. The Dermatoglyphics pattern is caused by primary ridge creation and an increase in the number of ridges from neighbouring ones.5
Cleft lip and palate are the second most common birth defects. Sometimes it can occur only as a single cleft lip/cleft palate or as a combination of both. In India, cleft lip and palate occurs approximately 1.4 per 1000 live births and a marked racial variation is seen in the incidence of Cleft lip and palate.6 In the literature, it has been shown that there is a connection between clefts, malocclusions, and abnormalities in the affected person's dermatoglyphics. This information sheds light on the relationship between craniofacial anomalies and dermatoglyphics and helps us forecast when clefts are likely to arise in the future. It has been conclusively proven in the study that in cases with hereditary cleft lip/palate, the predisposition for malocclusion and clefts begins in the previous generations itself. The dermal patterns may phenotypically change as a result of this partial genetic penetration. It is believed that blood vessel-nerve pairs at the border between the dermis and epidermis during foetal development have an impact on the finger ridges. The location of sweat glands, changes in epithelial growths, and insufficient oxygen supply are only a few of the variables that may have an impact on the ridge patterns.7
Dermatoglyphics can be used as a cost-effective tool for the early identification of malocclusion and other orofacial complex disorders and thus as it is a non-invasive method therefore it provides a good patient compliance. Early identification can help the physician foresee children's oral issues and start early preventative and protective dental procedures. In underdeveloped nations with large populations and constrained health expenditures, dermatoglyphics can be incredibly beneficial for the quick, simple, inexpensive, non-invasive identification of groups at high risk of developing malocclusion and for prompt prevention. 8 Individuals with an initial diagnosis of a cleft lip/palate can be easily assessed with Dermatoglyphic pattern beginning in infancy and followed up until all management. 9 The objective of this study was the assessment of correlation of Dermatoglyphics with sagittal skeletal discrepancies and oral clefts. Based on the results of this study it may be possible to make better choice of investigation aid at a very early age as well as making a new innovation in providing the non-invasive and easiest aid for diagnosis of malocclusion and cleft patients.
Materials and Methods
For sagittal skeletal discrepancies
Inclusion criteria
Digital lateral cephalograms.
Patients with skeletal malocclusion I, skeletal malocclusion II, skeletal malocclusion III.
Patients who had not undergone any previous orthodontic treatment or oro-maxillofacial surgery.
Patients of 12-25 years of age.
Patients having no history of craniofacial trauma.
Method used for sagittal skeletal discrepancies patients
Pre-treatment digital lateral cephalograms of thirty patients were used which reported to the Department of Orthodontics & Dentofacial Orthopaedics at Career Post Graduate Institute of Dental Sciences & Hospital (CPGIDS&H), Lucknow. Due consent was taken from all the participants taking part this in-vitro clinical study. The patient cephalograms were recorded in natural head position, in which each patient was directed to stand at ease while the head was adjusted without using any external reference. Each patient was asked to not move their head & to bite lightly on their teeth while the radiographs were taken. Cephalometric tracing was done on digital cephalometric radiographs with an acetate matte tracing paper by conventional method. The radiographs were then divided into three groups after evaluating the inclusion and exclusion criteria which were as follows: Skeletal class I, Skeletal class II and Skeletal class III, respectively. The sagittal jaw relation was determined from the patient’s lateral cephalogram with assessment of the following parameters: SNA, SNB, ANB, Wit’s appraisal, condylion to Point A, condylion to gnathion, angle of convexity and facial angle (Steiner’s, Down’s, McNamara and Wit’s Appraisal).
Patients were requested to wash their hands with soap and water and wipe them with ethyl alcohol to remove perspiration, oil, and filth from the skin's surface before the Cummins and Midlo procedure was used to collect their dermatoglyphics. The ink stamp technique was used to capture the fingerprints. Both hands' dry distal phalanges were rolled on an ink pad and imprinted onto the paper that was secured in position using tape (Figure 1). The fingers were numbered from 1 to 5 from the left thumb to little finger and from 6 to 10 from the right thumb to little finger (Figure 2) to prevent fingerprint duplication. All of the fingerprints were checked for accuracy. The frequency of Arches, Loops, and Whorls was evaluated in the acquired prints.
Method used for cleft patients (lip/palate or combination of both)
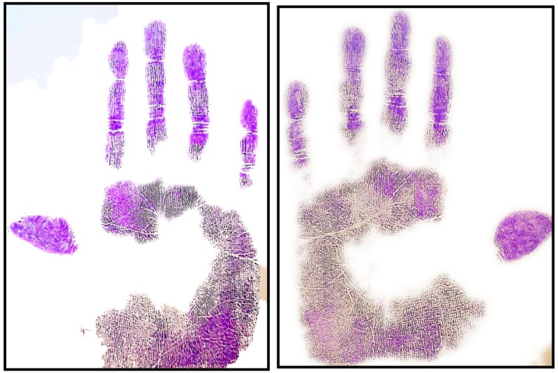
Intraoral and extraoral evaluation of ten cleft patients was done clinically. Dermatoglyphic patterns were taken after evaluating the inclusion and exclusion criteria. Duplicating ink was applied to the patients' palms before being pressed onto a sheet of paper that had been kept firm. Where the hollow of the palms had not yet contacted the paper, a sponge was placed under the paper on top of which the inked palm was pressed (Figure 3). The patterns were interpreted in accordance with Cummins and Mildo & Penrose.
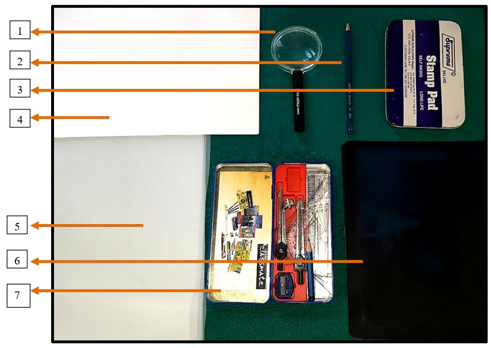
Armamentarium used
Magnifying glass
4h pencil
Stamp pad (97*160mm)
Bond paper
Acetate matte tracing paper
Digital lateral cephalograms
Geometry box (Figure 4)
Results
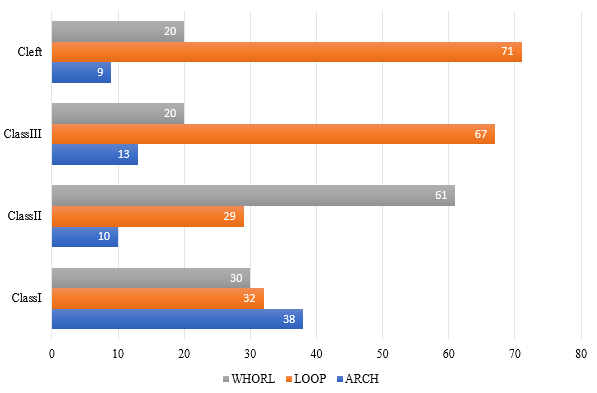
The data collected were analysed using the Statistical Package for Social Sciences for Windows (SPSS V27 Inc., Chicago, Illinois, USA). The skeletal values for categorization of sagittal skeletal discrepancies are summarized in Table 1 and the percentage distribution of the Dermatoglyphic patterns recorded from the 10 fingers of the studied subjects (N=40), classified into four groups, is formulated in Table 2. The dermatoglyphic results that were noted among the 4 groups showed a significant 38% of Arch pattern prevalent in the Class I subjects, 61% of Whorl pattern in Class II subjects, 67% of Loop pattern in Class III subjects and 71% of Loop pattern in Cleft subjects (Table 3 and Figure 5). The percentage distribution of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the 10 fingers (N=40) were evaluated for their significant association based on Fisher’s exact test and are recorded in Table 4, Table 5, Table 6, Table 7, Table 8, Table 9, Table 10, Table 11, Table 12, Table 13. Furthermore, Chi-square test indicated a statistically significant (p<0.001) association between the dermatoglyphic patterns and sagittal skeletal discrepancies and clefts, more than 54% of Class I subjects showed a positive correlation with Arch pattern, 33 % of Class III subjects and 35% of Cleft subjects indicated Loop pattern prevalence, whereas 46% of the Class II subjects showed a high tendency for the Whorl pattern of dermatoglyphics, respectively (Table 14).
Figure 2
All the fingers were numbered from 1 to 5 (left thumb to little finger) and from 6 to 10 (right thumb to little finger) to avoid fingerprint duplication.
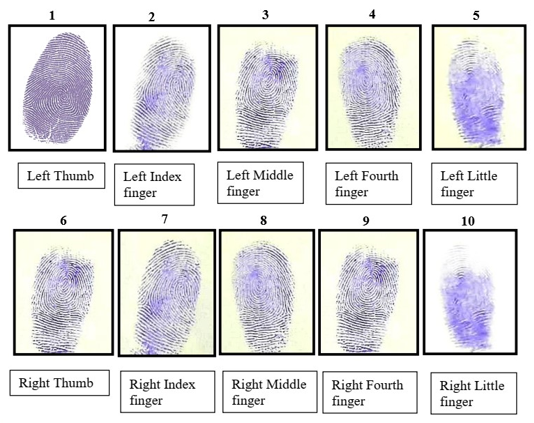
Table 1
Summary statistics of Parameters (Mean, Min, Max) of sagittal skeletal discrepancies.
Table 2
Percentage distribution (N%) of the Dermatoglyphic patterns recorded from the 10 fingers of the studied subjects (N=40), classified into four groups.
Table 3
The percentage distribution (N%) of Dermatoglyphics in different categories.
|
Category |
Arch |
Loop |
Whorl |
|
Class I |
38 |
32 |
30 |
|
Class II |
10 |
29 |
61 |
|
Class III |
13 |
67 |
20 |
|
CleftCC |
9 |
71 |
20 |
Table 4
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Left Thumb (N=40).
Table 5
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Left Index Finger (N=40).
Table 6
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Left Middle Finger (N=40).
Table 7
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Left Fourth Finger (N=40).
Table 8
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Left Little Finger (N=40).
Table 9
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Right Thumb (N=40).
Table 10
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Right Index Finger (N=40).
Table 11
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Right Middle Finger (N=40).
Table 12
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Right Fourth Finger (N=40).
Table 13
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the Right Little Finger (N=40).
Table 14
The percentage distribution (N%) of the Dermatoglyphic patterns within the three groups of sagittal skeletal discrepancies and clefts for the 10 Fingers (N=40).
Discussion
The development of occlusion occurs as an interaction and synergism of genetic and environmental factors. According to the functional matrix theory of Moss and Salentin (1969), genetic information is in the neurological, muscular, and neuromuscular fields, which indirectly influence the skeleton. 2 With evolution in every field of dentistry there is a need for development of a non-invasive, easy, and comfortable diagnostics aid in the field of orthodontics which should be added so that there can be easy diagnosis of skeletal discrepancies and oral clefts in orthodontic patients. Preventive or at a later interceptive methods can be applied for the developing/ developed malocclusion so that the patient social and mental wellness should not get affected. Different studies were being done to correlate the Dermatoglyphics with sagittal skeletal discrepancies and clefts. However, no combined study has been done for showing the correlation of sagittal skeletal discrepancies and oral clefts. Many quantitative and qualitative methods have shown great resemblance between these three factors: sagittal skeletal discrepancies, oral clefts and Dermatoglyphics as highlighted by the relationship between the Cleft lip/palate and Dermatoglyphics, reported by Woolf and Gianas (1976) 10 and Babler (1991). 11
Twenty-five North Indian men were the subjects of a research by Kharbanda et al (1982) 12 on real mandibular prognathism, which was validated by cephalometric Down's analysis. This was contrasted with the results of Dermatoglyphic analysis on those who had Class I occlusion and craniofacial pattern. According to their study, the craniofacial skeletal Class III pattern was linked to an increase in arches and ulnar loops at the expense of whorls on all digits other than digit II, as well as an increased frequency of whorls and radial loops and carpel loops on the interdigital area of palms. Also, the dermatoglyphic patterns of 311 kids with cleft lip, alveolus, and palate who had no other outward deformities were examined by Kanematsu et al (1986). 13 These tendencies were contrasted with those of the typical children. They discovered that genetic influences during the embryonic phase were responsible for the aetiology of the defects in the appearance of finger and palm prints.
The fingerprint patterns of 20 hypodontia patients were examined by Lakshmi (1989) 14 and compared to those of 20 normal males and 20 normal females. In people with hypodontia compared to normal females, the frequency of whorls and arch patterns was higher than that of loop patterns. In comparison to normal men, there was a higher frequency of whorls and a lower frequency of loops and arch patterns. Similarly, In comparison to controls, Balgir R. S. (1993) 15 found that individuals with cleft lip with or without cleft palate had an increased frequency of ulnar and radial loops, then arches, then whorls. This study, which found that loops occur more frequently than arches and whorls, is consistent with our own. Garima et al in (2015) 2 conducted the study and showed increased tendencies toward high frequencies of whorls in subjects. Their results were cognitive with the findings of present study as the whorl pattern was frequently observed in patients with Class II malocclusion, especially in thumb.
In a study by Matthew L. et al. (2005), 16 it was found that individuals with oral clefts had an increased frequency of ulnar loops, which was found to be highly significant. This was observed when comparing the fingerprint patterns on the distal phalanges of the ten fingers of fifty children with oral clefts to those of fifty normal children in accordance with the findings of our study as the correlation between the loop pattern and oral clefts patients on left thumb, left index finger and left fourth finger was recorded. Jaskiran et al in (2016) 8 conducted a study and showed an increased distribution of whorl pattern in Class II malocclusion. Their results were cognitive with the findings of present study.
The study, done by Sushma et al. (2017), 3 found that there was no unique pattern in Class I malocclusion, but that whorl pattern distribution was more common in Class II malocclusion and loop pattern distribution was more common in Class III malocclusion. Out of 10 fingers, the left thumb, left index finger, and left fourth finger were acquired (p-value < 0.05), which is consistent with the findings of our study. The study, which was carried out by Reddy et al. (1997),17 employed Dermatoglyphics to predict and contrast Class I, Class II division 1, division 2, and Class III malocclusion. According to the study, Class II division 1 and division 2 of the craniofacial system were associated with increased frequency of arches and ulnar loops and decreased frequency of whorls, whereas in the present study, Class II malocclusion was associated with increased frequency of whorl pattern and Class III malocclusion with increased frequency of loop pattern.
Dermatoglyphic patterns of individuals with normal occlusion and various grades of malocclusion were analysed and compared in a study by Trehan et al. (2000) 18 According to the study, radical loops and arches are more common in Class I and Class II division 1 malocclusions. In addition, compared to normal occlusion, an increased frequency of whorls was associated with Class I and Class III malocclusion, whereas in the current study, Class II malocclusion was associated with an increased frequency of whorl patterns and Class III malocclusion was associated with an increased frequency of loop patterns. A comparison of the Dermatoglyphics patterns of people with normal occlusion and various kinds of malocclusions was made by Reddy et al. (2013). 19 Some fingerprint patterns, like twinned loops, were observed with an increased frequency in Class II malocclusions and radial loops were absent in Class III malocclusions, whereas in the present study, whorl pattern was observed with an increased frequency in Class II malocclusion and loop pattern with an increased frequency in Class III malocclusion, which was contrary to the previous study's findings. Furthermore, twenty-four patients with ten Class I, eight Class II, and six Class III malocclusions participated in pilot research by Rajput et al. (2014). 20 Both quantitative and qualitative evaluations of the gathered dermatoglyphic patterns were conducted. The study showed that Class I malocclusion patients had an increased frequency of whorls, whereas Class II and Class III malocclusion patients had an increased frequency of loops. However, in our current investigation, there was no frequent distribution of whorl pattern in Class I malocclusion. There were no notable dermatoglyphic patterns of any kind in Class I malocclusion, however there were more whorl patterns in Class II malocclusion and more loop patterns in Class III. The variation in the results from the previous conducted studies can be explained by several limiting factors, such as the distinction in test design, no precise method for evaluating Dermatoglyphics and sagittal skeletal discrepancies and oral clefts, difference in the sample size and distribution and the variation in the methodology, execution and armamentarium used in the study, thereby affecting the final outcome of the study.
Conclusion
Patients are more likely to seek out orthodontic treatment now than ever before, with the primary goals being occlusion improvement and aesthetics. For the detection of sagittal skeletal discrepancies (malocclusion) and mouth clefts, a number of non-invasive diagnostic procedures have been developed, including the roentograph, orthopantomogram, and cervical vertebrae maturity indicator. The changed Dermatoglyphics (fingerprints) are frequently a reflection of the impact of heredity and environmental influences on early development and is therefore an acceptable non-invasive technique for the early detection of sagittal skeletal discrepancies and mouth clefts. The results of this study were in support of Dermatoglyphics showing the significant (p<0.05) correlation with sagittal skeletal discrepancies and oral clefts. Although malocclusion based on Dermatoglyphics can be predicted with a fair degree of accuracy, however it cannot be relied upon as a sole factor due to variations in the ethnicity and races, congenital, environment, and many other local factors.