- Visibility 97 Views
- Downloads 13 Downloads
- DOI 10.18231/j.jdp.2023.041
-
CrossMark
- Citation
Implant supported overdenture- Drifting from the conventional approach
- Author Details:
-
Maithilie Aggarwal
-
Neeta Pasricha *
-
Shuja Mohammed Khan
-
Siddhi Tripathi
Introduction
Patients and clinicians face a variety of difficulties when a patient goes from having no teeth to having all of them, particularly in the mandible where bone resorption must be taken into account during prosthodontic rehabilitation.
Edentulous mandible patient has several treatment options: Fixed prosthesis- FP1, FP2, FP3 or the removable prosthesis- RP4, RP5. After following proper treatment planning and taking into consideration the finances of the patient we choose the appropriate treatment option. [1], [2], [3], [4]
This case report discusses the prosthetic rehabilitation of an edentulous patient using implants and fabricating an implant supported overdenture with O-rings and ball attachments. [5]
Case Presentation
A 66-year-old male patient came to the Department of Prosthodontics and Crown and Bridge with a chief complaint of missing teeth in upper and lower arches for 8 years. History of multiple uneventful extractions was reported 8 years back due to mobility of teeth. Last extraction was done in upper front region 5 years back.
Extra-oral examination revealed orthognathic facial profile with competent lips with medium length and moderate thickness that provides sufficient support.
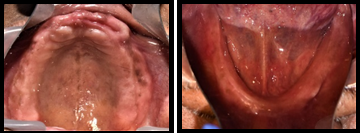
On intra-oral examination, patient had completely edentulous arches. Mandibular ridge was U-shaped with a low well-rounded contour. Ridge relation was class 1 with an inter ridge distance of 20 mm ([Figure 1]). As patient was seeking improvement in his facial appearance, a treatment plan was formulated for maxillary and mandibular implant supported overdenture after an informed consent was taken from the patient. An orthopantomogram was taken to gather comprehensive diagnostic information.

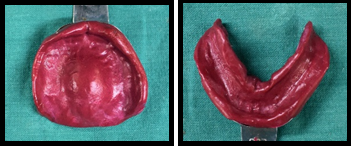
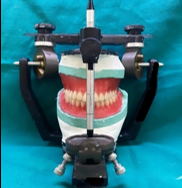
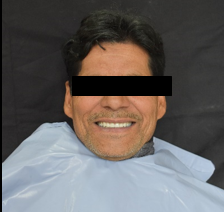
Preliminary impression ([Figure 2]) was recorded with impression compound (DPI pinnacle) and definitive impressions were made using low fusing impression compound (DPI pinnacle) and zinc oxide eugenol (DPI Impression Paste) in conventional manner. Jaw relation was recorded along with face bow transfer onto the semi-adjustable articulator ([Figure 3]). Teeth arrangement was done and evaluated as per the phonetics and esthetics ([Figure 4]).
After denture delivery was done and adjustments made in the patient’s mouth. The fabrication process includes of an implant supported overdenture with 2 implants in the B and D position (Misch classification). This type of overdenture prosthesis comes under the RP5 prosthesis and is classified as the OD-1. This prosthesis requires placement of implants in the mandibular lateral incisor region bilaterally at the same height of the crest and these implants are not splinted by a bar.
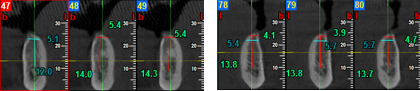
Radiographic markers (Gutta percha) were placed at the B and D region of the mandible according to the Misch classification to check the exact position of implant placement on the CBCT that followed. A CBCT was conducted to evaluate the bone quality ([Figure 5]).
Surgical phase
A two stage implant surgery was performed and two implants placed at B and D region of the mandible according to the Misch classification. The denture that was fabricated was used as a surgical guide to orient the implants in the correct position while drilling.

After implant placement and primary closure was obtained ([Figure 6]). The denture was given as a temporary prosthesis to the patient till osseointegration was complete. The implants were left for osseointegration for 3 months.

After 3 months, stage II surgery was done and gingival formers were placed for 14 days (figure 7). After that, ball attachments male components were placed on the implants ([Figure 8]).

The metal housings were then placed on the ball attachments and the metal housings were picked up on to the patient’s denture, that was fabricated earlier, by the direct pick-up method ([Figure 9]). Latex glove separator was placed on male attachments and housing with O rings was placed above it.

The denture was then delivered to the patient by checking the occlusion in both centric and eccentric planes. The implant supported overdenture was then finished and polished ([Figure 10]). The patient was kept on a regular follow up.
Discussion
There are two approaches to designing the implant-retained overdenture. The first method involves splinting implants with a stiff connecting bar that has an attachment mechanism built in to hold the overdenture in place. In the alternative method, an abutment with an integrated retentive mechanism provides the retention mechanism the implants are not attached to one another. The fact that the freestanding implants enable the use of prefabricated stock retentive abutments is one of their main advantages. [6], [7]
The use of implant bar raises the cost of treatment because it necessitates additional laboratory and clinical procedures for its production. The fact that the abutment itself is readily replaceable in the event of abutment failure is another benefit of prefabricated stock abutments. Remaking the overdenture is not necessary when replacing stock abutments because they are similar. On the other hand, replacing the implant interconnecting bar typically necessitates replacing the overdenture in the event of failure. [8]
The ball and o ring attachment system consists of a titanium male unit and an easily replaceable rubber-ring female unit that is retained in a metal retainer ring. It transfers the amount of stress to the abutments and provides an excellent shock resorbing effect during function. A distance of 10–12 mm from the crest of the ridge to incisal edge is the ideal interridge distance required for placement of this type of attachment system.
Conclusion
An implant-retained overdenture is one of the more straightforward and affordable alternatives for treating an edentulous mandible. Even though this treatment is widely accepted, there are still some disagreements on the best ways to fabricate overdentures, choose the right attachment mechanism and design the overdenture. Dental technicians and clinicians must follow good design principles, which include cost management, ease of maintenance and repair, and simplicity in manufacture. Enhances overall satisfaction and nutritional status, but also eases the fabrication and cost effectiveness over conventional removable prosthesis.
Source of Funding
None.
Conflict of Interest
None.
References
- RR Resnik. . Contemporary implant dentistry. 4th edn. 2021. [Google Scholar]
- HR Shafie. . Clinical and Laboratory Manual of Implant Overdentures 1st Edn. 2013. [Google Scholar]
- CE Misch. . Dental Implant Prosthetics. 2nd edn. 2014. [Google Scholar]
- DUK Jha, MK Singhal, C Nair, GN Dubey, A Agarwal, SK Badiya. An Evaluation of Attachments: Implant-supported Overdentures. J Dent Sci Oral Rehab 2016. [Google Scholar]
- S Patel, P Sutariya, H Shah, H Upadhyay, M Pathan, R Shah. Mandibular implant-supported overdenture: A systematic review and meta-analysis for optimum selection of attachment system. J Indian Prosthodont Soc 2021. [Google Scholar]
- GA Borges, RC Costa, BE Nagay, MB Magno, LC Maia, V Barão. Long-term outcomes of different loading protocols for implant-supported mandibular overdentures: A systematic review and meta-analysis. J Prosthet Dent 2021. [Google Scholar]
- AYP Wigianto, Y Ishida, T Matsuda, T Goto, M Watanabe, T Ichikawa. Novel Magnetic Attachment System Manufactured Using High-Frequency Heat Treatment and Stamp Technique: Introduction and Basic Performance. Dent J (Basel) 2022. [Google Scholar] [Crossref]
- R Hariharan, R Maniamuthu. Fundamentals of implant overdenture-overview. Online J Dent Oral Health 2021. [Google Scholar]
How to Cite This Article
Vancouver
Aggarwal M, Pasricha N, Khan SM, Tripathi S. Implant supported overdenture- Drifting from the conventional approach [Internet]. J Dent Panacea. 2025 [cited 2025 Sep 04];5(4):193-196. Available from: https://doi.org/10.18231/j.jdp.2023.041
APA
Aggarwal, M., Pasricha, N., Khan, S. M., Tripathi, S. (2025). Implant supported overdenture- Drifting from the conventional approach. J Dent Panacea, 5(4), 193-196. https://doi.org/10.18231/j.jdp.2023.041
MLA
Aggarwal, Maithilie, Pasricha, Neeta, Khan, Shuja Mohammed, Tripathi, Siddhi. "Implant supported overdenture- Drifting from the conventional approach." J Dent Panacea, vol. 5, no. 4, 2025, pp. 193-196. https://doi.org/10.18231/j.jdp.2023.041
Chicago
Aggarwal, M., Pasricha, N., Khan, S. M., Tripathi, S.. "Implant supported overdenture- Drifting from the conventional approach." J Dent Panacea 5, no. 4 (2025): 193-196. https://doi.org/10.18231/j.jdp.2023.041
