Introduction
Pediatric injuries involving the facial bone are associated with severe injury and trauma.1 Trauma is one of the leading causes of morbidity and mortality in children. Although less, maxillofacial fractures contribute to an important part of morbidity in children if not treated properly. These fracture patterns and mechanism of injury varies with age. Facial fractures in children differ from adults in anatomy and development, diagnosis, management and follow-up.2 Facial trauma in a growing child poses a considerable management challenge to the surgeon and an emotional burden to the patient and the family. 3 Here the management of this pediatric maxillofacial trauma study is limited to a single government educational institution in the rural area of Tamil Nadu.
Study design
The study data consists of facial traumatic fractures and associated soft tissue injuries in a rural medical college in Tamil Nadu reported during the period February 2017 to May 2018. Totally 19 cases (range 6-16 years of age) were reported out of which the majority are soft tissue injuries. Nine cases sustained bony injury. One of them was not willing to treatment and was managed with liquid diet antibiotics and analgesics. ORIF was done for 4 facial bony injuries two patients managed with MMF and two patients with Dental splints including arch wires and composites. The conservative approaches in the treatment of pediatric facial fractures are more common due to the presence of tooth buds and the elasticity of the pediatric bone.4 Simple splinting or intermaxillary fixation is used as a standard treatment for children with facial fractures in deciduous dentition. Convincing the parents to surgical procedures was difficult due to illiteracy and low socioeconomic status. In this study, open reduction and internal fixation were limited to microplates and mini plates. Orthodontic hard stainless-steel wires were also used in two cases.5 We were not able to use absorbable plates in this population because of cost factor. Here we present a case series of six patients who have been managed with minimal to maximum intervention and have given consent for photographs.
Case Reports
Case 1
A 12-year-old boy reported trauma in the maxillofacial region with facial soft tissue injuries and maxillary hard tissue injuries. He had an RTA with motor vehicle injury traumatizing his facial bones, forearm and leg. He had his plating done for his forearm injury. For his facial injuries, maxillofacial intervention was needed. He had severe soft tissue injury involving forehead, cheeks, lips and chin. Intra-oral examination revealed a severely displaced alveolar segment in the maxilla involving the right permanent central incisor and lateral incisor. The incisors were displaced 180˚ in the coronal plane impinging the upper lip. Occlusion was deranged with an inability to open the mouth due to severe soft tissue injury.
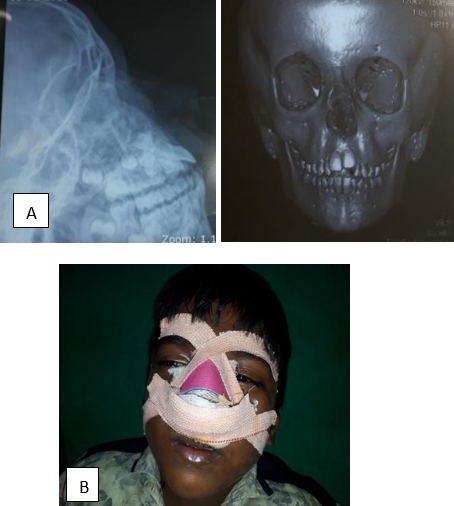
Diagnostic OPG and segmental intraoral periapical radiographs were taken to visualize the anatomy and the nearby developing structures (Figure 1A). Treatment started with debridement of injured soft tissue and bony injury. Controlled conservative excision-debridement was done for Facial soft tissue injuries and was repaired primarily. Reduction of the fractured and displaced segment was done and immobilization of the upper arch was done with the Ehrlich arch bar and orthodontic arch wires were also used6 (Figure 1B) IMF was done later and kept for six weeks to attain proper occlusion. The patient was reviewed after three years with the full set of permanent dentitions in occlusion, the maxillary incisors were nonvital with no root resorption for which root canal treatment was planned.
Case 2
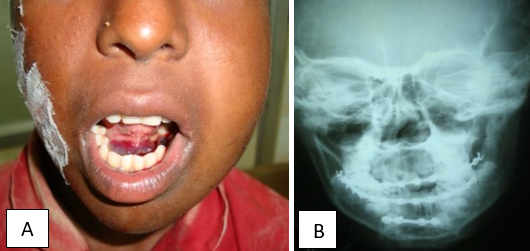
A male child 8 years old had an alleged history of road traffic accident while riding in the backseat of a two-wheeler and sustained injury to his face. History revealed loss of consciousness for five minutes and no vomiting or ear bleed. On examination patient had multiple abrasion and swelling on the left side of his face and chin and difficulty in opening the mouth. Tenderness over the right para symphysial region and occlusal difficulties. CT revealed a right mandibular para symphysial fracture and occlusion was not deranged (Figure 2A). Neurosurgical opinion was sought to rule out neurological injuries. Since the patient was in mixed dentition acrylic dental splint was made for both the arches and IMF (Figure 2B). In view of the age, mixed dentition and occlusal difficulties, the patient was put on a liquid diet initially and changed to a soft diet. The splint was kept in place for 3 weeks. The patient was reviewed and mouth mouth-opening exercises were given and proper occlusion was attained.
Case 3
An 8-year-old male child reported to our department with a history of self-fall from a height resulting in injury of the external nose. There was no history of loss of consciousness or vomiting. On examination dorsum of the nose was not in midline, contusion was present on the nasal bridge, the nasal septum deviated to the right side and there was nasal obstruction on the right side. There was no septal hematoma and no post-nasal bleeding. The patient was neurologically stable and there were no other serious injuries. X-ray of nasal bones and CT facial bones showed evidence of fracture of nasal bone with septal deformity (Figure 3A) After anesthetist evaluation child was taken for general anesthesia considering the extensive nature of the injury and age of and child. Closed reduction and moulding were done (Figure 3B). The patient was reviewed after a week.
Case 4
A 14-year-old girl presented with a history of falling from a wheeler and getting injured over the face. On examination patient had swelling over the left side of the face and chin and difficulty in opening the mouth. Intraorally patient had sublingual hematoma, tenderness over the right para symphysial region and deranged occlusion with no condylar injury (Figure 4A). Upper arch and lower arch Ehrlich arch bar placed and MMF was done. In the mandibular parasymphsial region plating was done with a four-hole SS plate and 1.5 mm screws (Figure 4B). Four to six weeks follow-up done. Proper occlusion was attained postoperatively with minor dental corrections.
Case 5
12-year-old male patient sustained a facial injury with hematoma and was managed conservatively. (Figure 5)
Case 6
An eight-year-old female patient had a trivial fall at home while playing and sustained soft tissue injury over the chin. The primary repair of the wound was done under LA. In the pediatric age group, these injuries can be managed with subcuticular closure and derma bond glue application. (Figure 6)
Discussion
Fractures in children are very rare because the bones are spongy and resilient. 1, 2 Soft tissue injuries are more common than hard tissue injuries in children. Boys are more affected than girls for maxillofacial injuries. 7 Causes of trauma in children are primarily due to motor vehicle injuries 3, 8 followed by sports-related injuries, accidental falls and violence. Patterns of facial trauma in children differ from adults by their anatomical distribution and developmental stage. 4 The diagnosis, management and follow-up of pediatric facial fractures have special characteristics and need specific knowledge. Management of such fractures in children belonging to rural areas needs more conservative methods of treatment and skills by the surgeon. 9 Patients are very anxious but at the same time conversion rate for fixing fractures is less because of illiteracy and poor socio-economic status. ORIF was done with minimal periosteal stripping4. Children tolerate MMF poorly. ORIF with plate success are seen better. Hard orthodontic stainless-steel wires and composite were also used for nonsurgical repositioning of fractured alveolar segments. Because of the cost factor, absorbable plates were not used in this rural population. 10 Children's compliance with cap splints was good.
Though complications of metallic fixation are more common in children due to growth concerns, we found no short-term growth abnormalities or facial asymmetry. The preliminary results were acceptable and complications did not occur in followed-up cases.
Limitation: Our study period was too short and the patient population is too small to determine the long-term effects of fracture treatment. Complications like tissue intolerance, growth restrictions and occlusal abnormalities were unable to be seen since continuous follow-up in these rural referral centres was poor. Patients who underwent minimal surgical procedures had good bone healing and less resorption patterns. However, a long-term observation is needed for children to study potential growth abnormalities.
Conclusion
Facial injuries with fractures of facial bones in children are uncommon but occur more frequently in major trauma like motor vehicle accidents and accidental fall injuries. Sports-related injuries are less common in the rural population. The most common being the fall injury damaging the dental hard tissue.
The anxiety factor, socioeconomic status of the parents, and children's skeletal and dental development play a major role in treating facial injuries in rural areas. Surgical procedures in children are not well-given concerns by parents in whom more conservative treatment with minimal surgical intervention holds good hope.
The greater osteogenic potential and faster healing rate in children help to treat with conservative therapeutic procedures and with minimal displacement of fractures. The stability of fixation in all four patients with facial hard tissue injury with minimal or no surgical intervention was high enough in this study group.
Anyhow long-term follow-up is needed to study and assess the facial growth development after trauma.