Introduction
The transverse growth usually completes before the vertical and sagittal growth. According to Gill et al. 8-18% of patients have maxillary transverse deficiency. Angell E (1860) was the first person to study transverse discrepancy and he proposed it as a skeletal deficiency of the upper jaw. Transverse changes present as solitary or in significance to other change and are of either skeletal or dentoalveolar in origin, but mainly are the results of a slight or severe constriction of the maxilla that leads to either unilateral, bilateral or unilateral functional crossbite and may be associated with Class III malocclusion or Class II malocclusion. 1
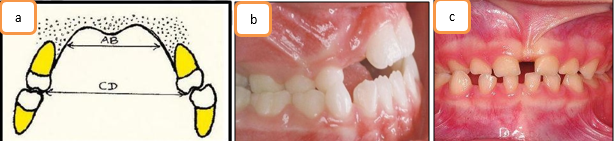
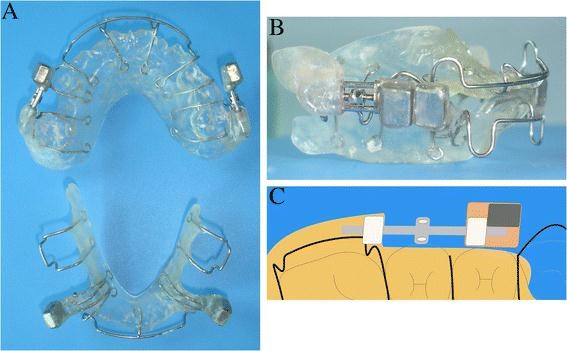
Etiology of TMD involves a combination of skeletal, dental or neuromuscular functional components. In fact malocclusion is a multifactorial phenomenon related to genetic, congenital, environmental functional or habitual origin (Figure 1a,b,c). Marshall et al.(2003) and Sayania et al.(2017) showed that mandibular molars have lingual inclination while eruption whereas maxillary molars have buccal inclination, while both of which follows straight path.(Sillman, 1964; Thilander and Lennartsson, 2002; Petrén and Bondemark, 2008). 2
The 3D images of study is used to measure palatal surface area and palatal volume (Oliveira De Felippe et al., 2008). Active maxillary expansion with an expansion plate is the classical method suggested for transverse discrepancy of maxilla (Petrén et al. 2003). An expansion plate with a midline screw in the deciduous dentition period cause skeletal (Melsen, 1975) compared to the use of an expansion plate in the mixed or permanent dentition stages 3 when orthodontic forces are considered only light enough to tip teeth (Ngan and Fields, 1995; Baccetti et al., 2001). Early corrections of functional problems should prevent adverse dental and facial development (Ninou and Stephens, 1994; Profitt, 2006, Ovsenik 2009; Melink et al., 2010). Ceylan et al. states that maxillary expansion can improve hearing ability. 4
The 3D images of study casts can be used to measure palatal surface area and palatal volume (Oliveira De Felippe et al., 2008). Although a considerable number of studies investigating the effects of correcting posterior crossbites have been conducted, the outcomes are very different (Petrén et al., 2003; Malandris and Mahoney, 2004; Harrison and Ashby, 2009). Maxillary expansion was reported to affect other different sutures.(Leonardi R, Sicurezza E, Cutrera A, Barbato E, 2023). 5
Diagnosis
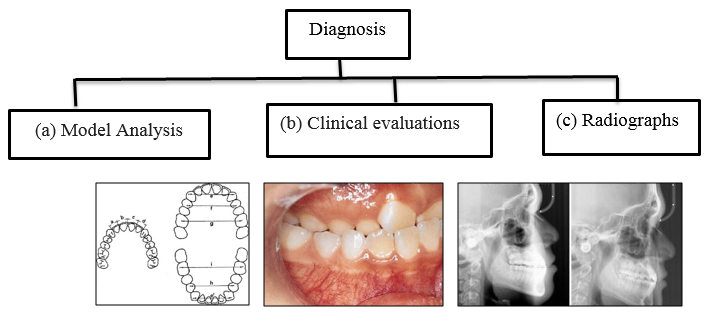
Because there are some changes in tissue from transverse maxillary hypoplasia, TDM is more difficult to diagnose than diagnosing vertical or sagittal disparity (Reyneke JP, Conley RS, 2020). The form and shape of the arch should be evaluated using the working model. This will allow specific measurements to evaluate changes in the maxilla (Rakosi, Jonas, Graber TM, 1993). There is extensive information about the diagnosis and procedures of maxillary defects. Confirmation was done through standard tests, clinical evaluation, and radiological evaluation. 6
Clinical evaluation
Crowding and protrusion
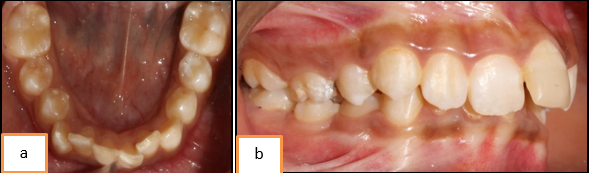
Crowding of lower arch (Figure 3a) and proclination of incisors (Figure 3b) are caused due to transverse discrepancy of maxilla. The reason is said to be due to discrepancies between the tooth size and the size of the alveolar base.
Intermolar width
Intermolar width measured between the points of the maxillary first molars (Figure 4). Normal molar width is in range of 35-39mm However, maxillary arches width lesser may be considered as crowded. 7
Crossbite
Crossbite is a clinical sign resulting from maxillary deficiency. Crossbite in posterior region is a common and valid indicator of transverse problems.
Radiographs
PA Cephalographs
A narrow maxillary intermolar without a crossbite also can indicate the need for maxillary expansion (McNamara, 2002). Vanarsdall and White says the dental arches are not an accurate means of assessing the transverse skeletal dimension.. Only the maxillary intermolar width correlates with the maxillary skeletal base dimension.9
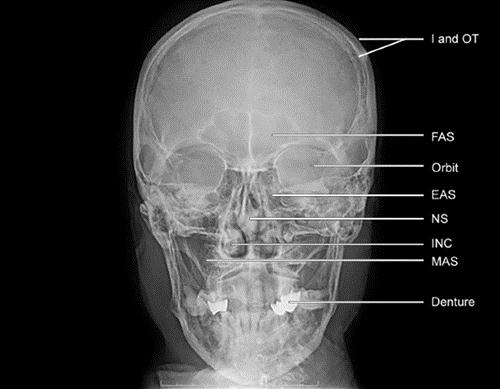
Radiographic identification and evaluation of transverse skeletal discrepancies should be done by using the postero-anterior (PA) cephalogram. PA cephalograms must be evaluated because growth in the transverse plane is completed earliest. Other methods of analysis were given by Grummons JCO 1987, Sassouni (1955) Bergman (1988) Betts (1994). 10
Radiographic assessment of midpalatal suture ossification
A viable midpalatal suture is considered highly responsive to forces acting in transverse plane, whereas a mature suture is unresponsive to nonsurgical expansion. but also is expanding under these circumstances, potentially is harmful to the alveolar bone and periodontium, and places teeth in potentially unstable bucco-lingual angulations. Melsen (1975) pioneered the combined use of detailed histology and microradiology to assess sutural changes in the human palate. Examining post-mortem palates from 33 boys and 27 girls aged 0–18 years, three stages in the midpalatal suture development. Stage one, the infantile stage, is notable for the wedging of the vomer between the two abutting palatal shelves(Y-shape configuration), In stage two, the juvenile stage, the upper portion of the Y flattens out and the vertical portion begins developing curve.. Last, stage three, the adolescent stage, is demarcated by the extensive interdigitation that generally is associated with full maturity. 11
Cone beam computed tomography
The maxilla is a complex bone that has fascinated anatomists for centuries. 3D radiographs are the only images from the past 524 years that surpass the master’s work (Banerji, 2012). Others consider da Vinci’s attention to detail a valuable lesson for clinicians in training, whose reliance on state-of-the-art diagnostic tools can lead to misdiagnosis if the machines are considered infallible (Gerrits & Veening, 2012).
Management
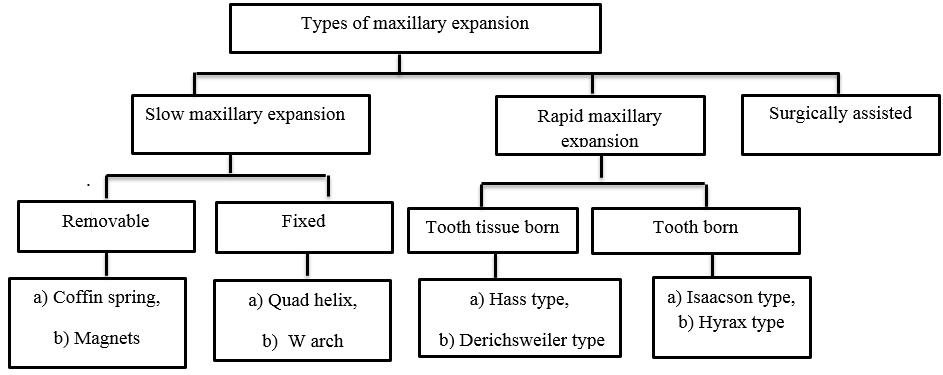
Maxillary expansion is the treatment of choice for the transverse discrepancies of maxilla. Orthodontic expansion or orthopedic expansion are two available options. Treatment modalities for expansion are: Rapid maxillary expansion (RME), Slow maxillary expansion (SME) and surgically assisted maxillary expansion. Every treatment modality comes with their respective pros and cons. Specialist should select any one available options depending upon specific individual patients need keeping in mind respective age and severity of malocclusion. 11
Slow Maxillary Expansion
Slow palatal expansion is a technique used to correct the narrow upper arch by increasing its width in transvers direction. Even if the enlargement is only dental, skeletal alterations are still noticeable. There is less tissue resistance in structures around the maxilla, and there is an increase in bone formation in the mid-palatine suture.1
Removable
Coffin appliance
Originally introduced by Walter Coffin–1875.
Design
This expansion device consists of a wire in the form of omega of 1.25 mm thickness, that is placed in the region of midpalatal raphae. Whose ending is covered into acrylylic which covers the palatal surface.12
Disadvantage
It requires that patients comply with activation and wear-time prescriptions. During expansion, failure to wear the appliance will usually result in rapid relapse.
Magnets
Magnetic forces for maxillary expansion were first described by Vardemon et al 1987.
Design and mode of action
Banded magnets produced more pronounced skeletal; versus overall expansion effects. The continuous force of 250-500 gm could generate dental and skeletal movements, the degree depending on patients status (age, growth, etc).13
Advantage
They impart measured continuous force over a long period of time, therefore the risk of external root resorption is decreased.
Disadvantage
They oxidized in the oral environment due to the potential formation of corrosive products which can be overcome by coating magnets. Magnetic appliances are bulky as they must be adequately stabilized and contain stout guide rods to prevent the magnets becoming out of line and causing unwanted rotational movements. 14
Fixed
Quad-helix appliance
The quadhelix appliance is a modified Coffin’s W-spring and was described by Ricketts. Four helices were incorporated into the W-spring helped to increase the flexibility and range of activation The Ricketts quad-helix appliance is used in expansion of dental and even mild skeletal deficiencies.12
Design
The quad helix can be used on acrylic blocks with occlusal overlays and even molar bands. The device is easy to use and works because it does not depend on the patient cooperation.
Mode of action
The quadhelix appliance works with a 6:1 ratio of buccal tipping and bony expansion in in prepubertal children.
Advantage
It does not depend on patient cooperation. This is helpful in molar derotation. Removable quad helices can be used to introduce buccal root torque on the upper molars.
Disadvantage
It is associated with molar tipping and bite opening. No orthopaedic change (although some orthopaedic change has been suggested in pre-adolescent children). Usually no more than 4 mm expansion achievable. 14
Rapid Maxillary Expansion
The main aim of the procedure is to separate the mid-palatine suture mechanically in the upper constricted arch, high palate, and complete crossbites. Rapid palatal expansion widen the narrow upper arch, but its impact is also seen on the bones of the head and face. An expansion (active) of 0.3 to 0.5mm occurs in the palate. Graber advocated Rapid Maxillary Expansion as a method to treat patients suffering from cleft lip and palate problems.11
Tooth tissue born rapid maxillary expansion
They consist of an expansion screw with acrylic abutting on alveolar ridges.
Hass type
The first descriptions of rapid maxillary expansion (RME) were made in 1860-61 by Emerson Angell and further developed and promoted by Haas. The Bonded RPE were first described by Cohen and Silverman in 1973. 9
Design
Hass expander and Hyrax expander are most commonly used and involves the first premolar and molar banding. The Haas expander has pads (acrylic) on palatal side so as to provide good bony anchorage. The lateral forces are directed indirectly onto the bone during early phases of expansion
Mechanism of action
According to Haas, is a rigid appliance that uses a jackscrew to extend in 10–14 days for maximum dental anchoring. The forces produced by this device are said to be in the range of 3–10 pounds, which is greatest orthopedic impact.
Advantage
It is easy to cement during the mixed dentition stage, when retention from other appliances can be poor. Number of appointments are reduced. There is reduced posterior teeth tipping and extrusion.
Disadvantage
Once the appliance is delivering a force in excess of the limit for orthodontic tooth movement, the sutures are opened and the teeth undergo minimal movement relative to their skeletal support. Heavy, rapid force on the posterior teeth does not allow for tooth movement to occur in time, transferring the force instead to the sutures.
Derichsweiler type
Introduced by Derichsweiler, 1953 is a tooth- tissue born rapid palatal expander.
Design
This fixed appliance is tooth tissue and tooth borne type of appliance and can also be banded. The molar and premolar are banded. Wires are tagged and soldered onto the palatal aspect of the band. Those wires tags are inserted into a split palatal acrylic plate, incorporating a screw at its center.9
Tooth born rapid maxillary expansion
They consist of only bands and wires without any acrylic covering.
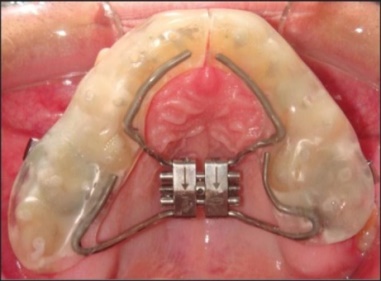
HYRAX expander
It is a tooth borne appliance, which was introduced by William Biederman in 1968.
Design
This type of appliance uses a special screw called HYRAX (Hygenic Rapid Expander). The Hyrax Expander is essentially a non-spring loaded jackscrew with an all wire frame. The screws uses heavy gauge wire extended to follow the palatal contours and soldered to premolar and molar bands.10
Mechanisms of action
Each activation of the screw produces approximately 0.2 mm of lateral expansion and it is activated from front to back.
Surgically Assisted Rapid Maxillary Expansion (Sarme)
Mechanism of action
SARME is a form of distraction osteogenesis. Where a partial osteotomy or corticotomy aids expansion with a tooth- or bone-born expansion appliance (Figure 16). Lagravère et al reported that the immediate intermolar width increased by 7.1−8.7 mm with a smaller intercanine width increase of 4.9−5.2 mm.
Newer Treatment Alternatives Over Conventional for TMD
Schwarz appliance
Schwarz appliance given by Artur Martin Schwarz (1887–1963).
Design
When space needs to be created for the teeth in crossbite, a simple Schwarz appliance with occlusal coverage will usually sufice.
NiTi expander
Inventor: Wendell V (Figure 18).
Archwire expansion
Another method commonly used by clinicians to attempt transverse correction is by expanding the upper archwire and contracting the lower archwire (Figure 19).
The Functional orthopedic magnetic appliance (FOMA)
Vardimon et al (AJODO 1990)" developed an intraoral intermaxillary appliance for the treatment of Class III malocclusions that exhibit mid face sagittal deficiency with or without mandibular excess.
Design
The FOMA will consists of upper and lower acrylic plates with permanent magnet incorporated into each plate.
Standard appliance Cap splint appliance
Design
The screw should be ideally mounted as high in the palatal vault as possible. The screw is mounted in the midline of the vault with the thread axis in line with the anterior borders of the first permanent molars.
Butterfly expander
A new rapid palatal expansion appliance, called a butterfly expander that they used to treat patients in the mixed dentition (Cozza, Giancotti and Petrosina, in 1946).
Appliance design
The butterfly expander has design similar to Haas appliance with modifications. A butterfly-shaped steel frame work incorporating high midpalatal jackscrews extends forward to the palatal surfaces of the deciduous canines. The appliance is soldered to bands on the second deciduous molars.
Mechanism of action
The appliance exerts forces on mid palatal suture to expand the two lateral halves of palatal on activation.
Conclusion
Many methods of diagnosis and eliminating transverse problems is discussed in this review article. Clinicians should be aware of associated pros and cons of each methods discussed here. The method chosen will depend on factors, like the type of the crossbite (dental or skeletal), the amount of dento-alveolar compensation, severity of the discrepancy, and growth of the patient. Consideration should be given to the stability of the correction and to the provision of adequate long term retention.14, 15, 16, 17