- Visibility 92 Views
- Downloads 2 Downloads
- DOI 10.18231/j.jdp.2024.019
-
CrossMark
- Citation
Enhancing orthodontic precision: A comprehensive review of temporary anchorage devices
Introduction
Temporary anchorage devices (TADs) have become a pivotal innovation in contemporary orthodontic practice, offering a reliable solution for achieving effective and predictable tooth movement. These small, screw-like implants, typically made from titanium or other biocompatible materials, are temporarily inserted into the alveolar bone to provide a fixed point of anchorage. This allows for precise application of orthodontic forces without relying on patient compliance or the need for extraoral devices.
According to Cope (2005), the introduction of TADs represents a paradigm shift in orthodontics, allowing for greater control and predictability in treatment outcomes.[1] Numerous studies have validated the effectiveness and safety of TADs. Papageorgiou, Zogakis, and Papadopoulos (2012) conducted a meta-analysis that demonstrated low failure rates and highlighted various factors influencing the success of miniscrew implants in orthodontics.[2] Furthermore, Poggio et al. (2006) provided detailed guidelines for the optimal placement of TADs, identifying "safe zones" in the maxillary and mandibular arches to minimize the risk of complications and enhance stability.[3]
In addition to their effectiveness in routine orthodontic cases, TADs have proven invaluable in complex treatments, such as the correction of Class II malocclusions. Papadopoulos (2014) discusses the versatility of TADs in providing skeletal anchorage, which facilitates significant orthodontic movements that would otherwise be challenging to achieve.[4] Moreover, Antoszewska-Smith et al. (2017) demonstrated through a systematic review and meta-analysis that TADs significantly improve anchorage control during en-masse retraction, leading to more efficient and effective orthodontic treatments.[5]
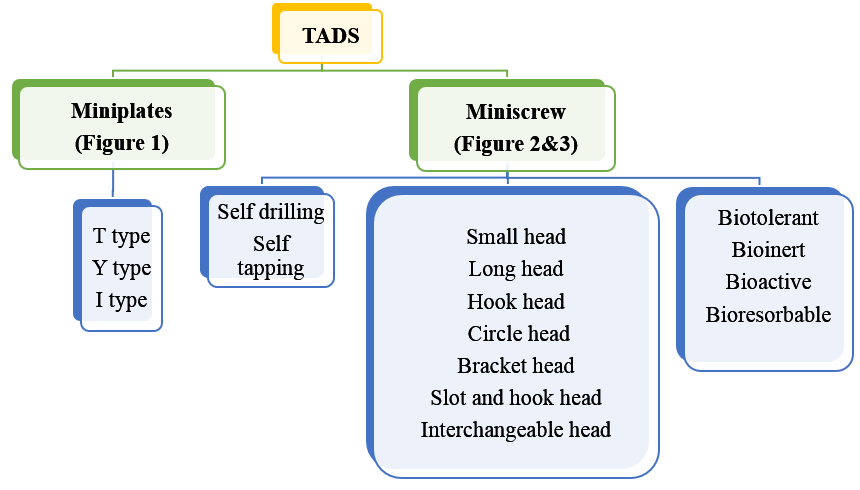

Materials Used for Implants
Titanium alloy, titanium-coated stainless steel, or bioinert pure titanium are the materials used in conventional MSIs (Miniscrew implants). Because of its established biocompatibility, the medical-grade titanium alloy is the one that is utilised the most frequently among these. Ti6Al4V, or grade V medical titanium, is the preferred material. It is an alloy of titanium, aluminium, and vanadium. In comparison to commercially pure (CP) titanium, it offers greater strength and biocompatibility. [6]
Understanding Implant Sites for TADS
Understanding the sites of implant placement ([Figure 5]) is crucial for ensuring the success of the procedure.
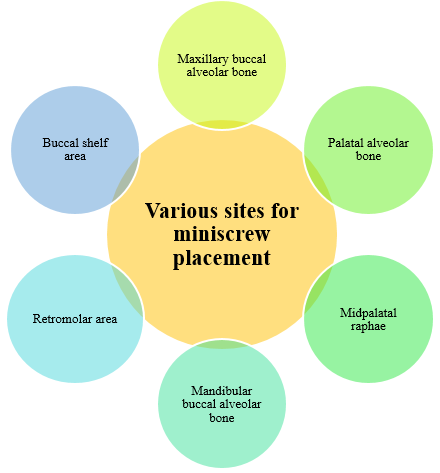
Maxillary buccal alveolar bone
It is the most common site for placing Temporary Anchorage Devices (TADs). A safe spot for miniscrew placement, with sufficient inter-radicular space, is located between the second premolar and first molar. [7]
Targeting the most apical region where the cortical bone is thick and dense, it is better to introduce TADs mesiodistally between the first and second molars for the best primary stability. However, the reduced inter-radicular space in this location poses a limitation. Although more apical placement may provide additional inter-radicular space, there is a risk of irritation and discomfort if a TAD is positioned in the movable mucosa. [8]
Maxillary palatal alveolar bone
The palatal cortical bone is thicker and denser than the buccal cortical bone. The thickest palatal cortical bone is located between the canine and first premolar, while the densest inter-radicular palatal bone is found between the first and second premolars. [9]
Midpalatal suture
In this region, due to the presence of thick and dense bone, pilot drilling is recommended prior to miniscrew placement. Additionally, due to the presence of thick mucosa in this area, longer TADs are preferred. An ideal location for miniscrew placement is 1–2 mm lateral to the mid-palatal suture particularly in growing patients. This is because of the presence of under-ossified bone and soft tissue at the suture site in growing individuals.
Mandibular buccal alveolar bone
The mandibular buccal inter-radicular space is largest between the first and second premolars and increases vertically from the cervical area to the apex. [10] The inter-root distance is also found to be greatest between the first and second molar, and noted that the cortical bone thickness tends to increase from the anterior to the posterior region.[11], [12] Theoretically, the denser cortical bone in the mandible should lead to a higher success rate for TADs compared to the upper arch. However, Park et al. found that the success rate of TADs was actually lesser in the mandible than in the maxilla. [13]
Buccal shelf area
If placing a Temporary Anchorage Device in the posterior inter-radicular area of the mandible is difficult, buccal shelf area of mandible offers a dependable alternative. This area is beneficial because it allows for the insertion of TADs with increased diameter parallel to the root, minimizing the risk of root injury. A high success rate of 93% for TADs placed at this site has been reported, with no significant difference in success rates whether they were positioned in movable mucosa or attached gingiva. [14]
Retromolar area
The retromolar area is another alternative site for implant placement. Although the success rate of TADs in the retromolar pad is quite high, there is a risk of injuring the lingual and inferior alveolar nerves if the TADs shift to the lingual side of the retromolar pad. [7]
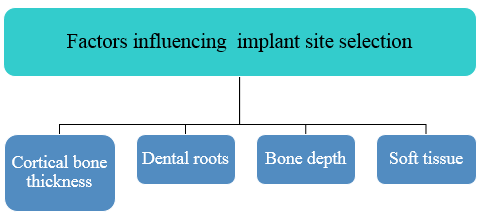
Factors Affecting Implant Site Selection
Several factors can influence the precise placement of an orthodontic mini-implant ([Figure 6]). The complexity of an insertion site depends on the number of anatomical boundaries present. Ideally, the mini-implant should be placed within the bone volume defined by these boundaries, ensuring that the screw interacts with only one boundary: the cortical plate in which it will be anchored. These boundaries influence the success rate of the mini-implant and the potential for complications. Therefore, a site with fewer boundaries is preferable to one with multiple boundaries. [8]
Cortical bone thickness
The cortical bone is crucial for providing stability to the mini-implant and is arguably the most critical anatomical factor to consider when selecting the placement location. A cortical plate that is too thin cannot offer adequate mechanical retention. Conversely, an overly thick plate is also undesirable. It is important to note that the thickness of the cortical plate affects the insertion torque at the implant site, with excessive torque potentially damaging the bone and causing late failures. Therefore, it is advisable to avoid both excessively thin and overly thick cortical bone for optimal implant stability. [15] The optimal range for achieving maximum success seemed to be between 1 mm and 1.5 mm. [16]
Dental roots
The proximity of the screw to the adjacent dental roots is the second most critical factor influencing the success of TADs. Generally, placing TADs closer to the roots increases the likelihood of screw failure. [17], [18], [19]
To reduce the risk of placing TADs too close to the roots, various strategies can be employed. For instance, anatomical averages can serve as general guidelines. These averages indicate that while buccal insertion space is often limited, several sites on the palate offer ample inter-radicular space. Notably, the area between the maxillary first and second molars provides a favourable inter-radicular distance. [3], [7], [11], [20], [21], [22]
Another consideration is to diverge the roots orthodontically in the sites that lacks adequate space of implant placement. [3]
Bone depth
Bone depth is the distance from the cortical plate, which provides screw retention (the first anatomical boundary), to the opposite cortical plate or another anatomical structure that may restrict insertion. [23]
Engaging or even penetrating the contralateral cortex generally does not raise the risk of screw failure. While single cortex engagement is standard and offers adequate retention for orthodontic purposes, some clinicians advocate for bicortical engagement in orthopedic applications, such as rapid palatal expansion (RPE) or protraction facemask use. [24]
Most perforations of the nasal cavity cause no issues, apart from possible discomfort or irritation. However, perforation of the maxillary sinus can lead to more serious complications due to inadequate drainage. [8]
Soft tissue
Attached gingiva refers to the gingiva located between the alveolar crest and the mucogingival junction. This area provides the most suitable soft tissue for mini-implant insertions because it is firmly attached and therefore remains stable, minimizing movement around the TAD. [25]
Various safe zones for implant placement are mentioned in [Table 1]
|
Safe zones for implant placement |
|||
|
Posterior region |
Anterior region |
Palate |
Other locations |
|
In both maxilla and mandible, MSI can be safetly placed between the roots of second premolar and first molar and between first molar and second molar through buccal cortical plate |
Maxilla - Between central and lateral incisors at an approximate distance of 6 mm from the CEJ |
The interradicular space between first and second premolar, second premolar and first molar, first molar and second molar |
Maxillary tuberosity |
|
|
One MSI can be placed in the midline just below the anterior nasal spine |
Midpalatal raphe - Non growing |
Infra zygomatic |
|
|
Mandible - Inter radicular bone between lateral incisor and canine |
Para-median position - 3 to 6 mm laterally and 6 to 9 mm posterior to incisive foramen |
Retromolar area |
|
|
|
|
Buccal shelf area |
Technique of Miniscrew Placement
Case selection
Proper medical history should be taken prior to miniscrew insertion – Patient having any systemic diseases affecting bone and patient under medication that affects bone metabolism.
Radiographs should be taken to evaluate the bone quality, inter-radicular space, crestal bone level, and mesio-distal angulation.
Informed consent
Oral cavity should be free from gingival inflammation and periodontal diseases. Oral prophylaxis and oral hygiene intructions should be given to the patient.
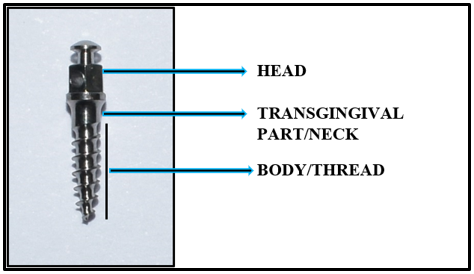
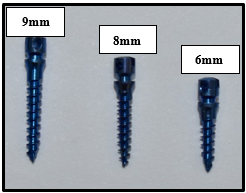
Miniscrew selection
Screw length
The miniscrews are available in the length of 5 to 12 mm. (Figure 6) Factors affecting the selection of miniscrew length includes;
Bone quantity and bone quality
Good cortical bone – Small screws can be used
Trabecular bone – Long screws might be needed
Minimum contact of screw with the bone should be 6mm in maxilla and 4 mm in mandible. So, the commonly used screw length is 7-8mm in maxilla and 5 to 7mm in mandible.
Soft tissue thickness
Thick soft tissue – Long screws should be used. Example – Thick mucosa covering palate usually requires long screws of 10-12 mm. However, in the Midpalatal suture the soft tissue thickness is less and small screw can be used in this area.
Screw thickness/Diameter
Available thickness – 1.2 to 2.7 mm.
The screw diameter is selected based on the inter-radicular space. A miniscrew intended to be placed between roots should be narrow enough to get accommodated and should have at least 1 mm bone around its maximum diameter.
Commonly used miniscrew thickness is 1.5mm. The miniscrew thickness of 1.2 mm is used between the lower incisors because of minimal inter-radicular space.
The primary stability of miniscrew depends mainly on screw thickness. [26], [27] However, there is no significant difference in the stability of TADS of greater than 1.5mm diameter and screw of greater than 2mm thickness was found to be less stable and might cause root injury. [28]
Miniscrew placement guide can be fabricated on a recent plaster model that helps in accurate placement of miniscrew.
Additionally, the patient is advised to begin taking 250 mg of amoxicillin or another appropriate antibiotic the night before the procedure. Patients who appear to be less pain-tolerant may also be given a safe painkiller one hour prior to the procedure.
The patient is asked to rinse with 10 ml of 0.12% chlorhexidine gluconate mouthwash for 1 min. [6]
Administration of local anaesthesia.
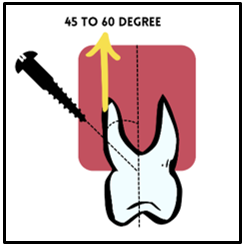
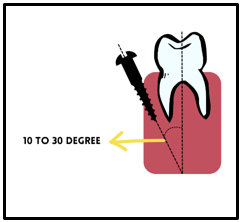
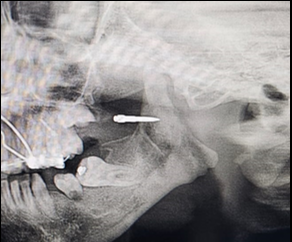
The maxillary buccal miniscrew (Self-drilling) is then inserted between the roots of premolar and molar at an angle of 45 to 60 degree ([Figure 8]) to the long axis of teeth and at an angle of 10 to 30 degree in the mandibular buccal region ([Figure 9]).
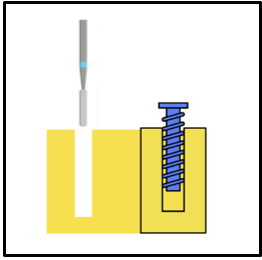
In case of self-tapping miniscrew, the pilot drilling is required before screw insertion ([Figure 10], [Figure 11])
A course of antibiotics, stringent oral hygiene care, and avoidance of hard meals would all be necessary during the postoperative phase to prevent damage to the miniscrew. It is possible to take the painkillers as needed.
After a week, there should be another follow-up to thoroughly examine for any symptoms of inflammation and mobility.
Loading of Implant
Research conducted at AIIMS examines the stability and peri-implant inflammation by analyzing the peri-miniscrew crevicular fluid (PMICF) and found that the inflammatory markers gradually decrease to baseline levels over a three-week period. Consequently, Dr. Kharbanda's protocol recommends delayed loading after three weeks. [6]



|
S.No. |
Miniplate |
Miniscrew |
|
1 |
More invasive |
Less invasive |
|
2 |
More expensive |
Less expensive |
|
3 |
Post-operative pain and discomfort present |
Less post-operative pain and discomfort |
|
4 |
No interference from dental roots as they are placed away from dental arch |
Inter-radicular placement might increase the risk of root damage |
|
5 |
Overall success rate is better than miniscrew. |
In situations when intermittent inter-arch elastic traction is employed, a single miniscrew is more prone to failure. |
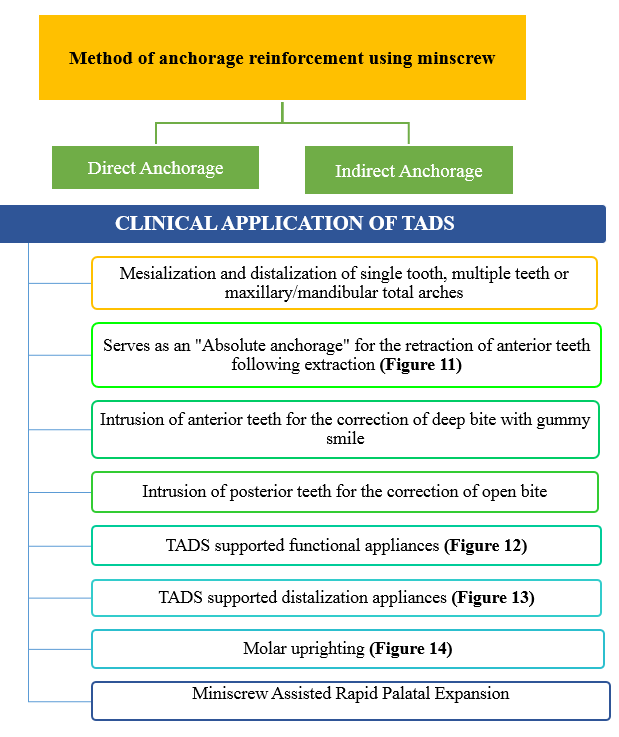
Clinical Application of TADS
Open bite treatment
For maxillary molar intrusion, miniscrews provide a dependable and minimally invasive solution. However, in scenarios where Surgically Assisted Rapid Palatal Expansion (SARPE) and posterior intrusion are simultaneously necessary, miniplates become crucial. This is because the anchorage units must be positioned above the osteotomy cuts. Additionally, for the intrusion of mandibular molars, miniplates are the preferred option. [29], [30], [31]
Class II treatment and molar distalization
For maxillary molar or arch distalization to correct Class II malocclusions, using miniscrew-supported distalizers in the anterior palate is a less invasive option. Therefore, anchorage miniplates, being unnecessarily invasive, should be reserved only for situations where placing a midpalatal miniscrew is not feasible. [32], [33], [34]
Class III malocclusion
In Class III correction, when the entire mandibular arch needs to be distalized, miniplates offer a notable advantage, particularly if the third molars must be extracted. Conversely, buccal shelf miniscrews present a viable alternative and involve less surgical intervention for placement.
Class III growth modification
In situations where maxillary protraction is needed, whether using a facemask or Class III elastics attached to mandibular symphysial miniplates, palatal miniscrews can be utilized instead of miniplates. This approach enables bone-borne expansion and protraction with minimal surgical intervention, which is particularly beneficial for young children. [35], [36], [37]
Intra-arch mechanics
Almost all intra-arch mechanics can be adequately anchored by miniscrews located in interradicular areas.
Advantages and Limiting Factors of Miniscrews and Miniplates for Orthodontic Treatment Miniscrews
Miniscrews
Force application
Miniscrews are capable of offering enough anchoring to facilitate orthodontic tooth movement. Miniscrews have been found to be capable of withstanding forces ranging from 300 g to 800g. [38], [39], [40], [41]
Advantages of miniscrews
Minimal cost
Ease of placement and removal
Adequate anchoring for tooth movement
Limiting factors of miniscrews
Root damage from miniscrews
One limitation on the location of miniscrew implantation is the possibility of causing harm to roots during the implanting process.[42] The use of a surgical template was suggested by Liu et al. [43] and Suzuki and Suzuki[44] as a way to avoid damaging roots when placing miniscrews. Cone-beam computed tomography can also yield valuable data for determining the cortical bone thickness and root-to-root distance. [17], [45] If a miniscrew damages a root and is removed right away, the damage to the dentin or cementum is likely to be limited, leading to nearly full recovery of the root surface. Normal healing won't happen, though, if the miniscrew penetrates the pulp.[46], [47], [48] Consequently, extra-alveolar placement of the minis crew is advised as having a high success rate to prevent root injury. [14], [49]
Fracture of the miniscrew
For patients with dense bone, predrilling [50] and the use of miniscrews larger than 1.5 mm in diameter are crucial for fracture prevention. [51]
The use of a trephine bur to remove a broken miniscrew removes a lot of surrounding bone; instead, use a carbide bur to remove the surrounding bone and a Howe plier to remove the damaged TAD. [52]
Ingestion of a miniscrew
A patient runs the risk of swallowing a miniscrew if it loosens while they are eating or sleeping. The miniscrews sharp point may become stuck in their stomach, but it usually comes out spontaneously. [53]
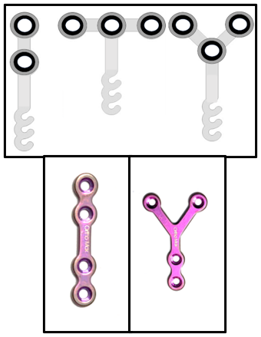
Miniplates
Miniplates are a solution to miniscrew drawbacks that were created by Sugawara and Nishimura. [54]
Force application
Maxillary protraction has been achieved with 300–500g of force on the maxilla using facemask and miniplates.[55], [56] To withstand the high forces required for orthopaedic therapy, miniplates are fastened with two or three screws.
Advantages of miniplates
Solid anchorage
High success rates
Low danger of fracture
Low possibility of root injury
Limiting factors
Post-operative pain and discomfort.
Cost is higher than miniscrews.[57]
Conclusion
In conclusion, TADs represent a significant advancement in orthodontic treatment, offering a reliable and efficient solution for achieving complex tooth movements. The minimally invasive nature of TADs, combined with their relatively low risk of complications and ease of placement and removal, makes them an appealing option for both practitioners and patients. The ability to avoid more invasive surgical procedures, such as orthognathic surgery, in certain cases adds to their value as a treatment modality. Their versatility, coupled with the potential for improved treatment outcomes and patient satisfaction, underscores their importance in modern orthodontic practice. As the field progresses, TADs will likely play an increasingly prominent role in helping orthodontists achieve precise and effective results for their patients.
Source of Funding
None.
Conflict of Interest
None.
References
- JB Cope. Temporary Anchorage Devices in Orthodontics: A Paradigm Shift. Semin Orthod 2005. [Google Scholar]
- SN Papageorgiou, IP Zogakis, MA Papadopoulos. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop 2012. [Google Scholar]
- PM Poggio, C Incorvati, S Velo, A Carano. Safe zones": A guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod 2006. [Google Scholar]
- MA Papadopoulos. . Skeletal Anchorage in Orthodontic Treatment of Class II Malocclusion: Contemporary applications of orthodontic implants, miniscrew implantsand mini plates. 1st Edn. 2014. [Google Scholar]
- J Antoszewska-Smith, M Sarul, J Łyczek, T Konopka, B Kawala. Effectiveness of orthodontic mini-implants in anchorage reinforcement during en-masse retraction: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 2017. [Google Scholar]
- OP Kharbanda. . Orthodontics: Diagnosis and Management of Malocclusion and Dentofacial Deformities. 3rd edn. 2020. [Google Scholar]
- J Park, HJ Cho. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am J Orthod Dentofacial Orthop 2009. [Google Scholar]
- JH Park. . Temporary Anchorage Devices in Clinical Orthodontics, First Edition 2020. [Google Scholar]
- H Ohiomoba, A Sonis, A Yansane, B Friedland. Quantitative evaluation of maxillary alveolar cortical bone thickness and density using computed tomography imaging. Am J Orthod Dentofacial Orthop 2017. [Google Scholar]
- KA Schlegel, F Kinner, KD Schlegel. The anatomic basis for palatal implants in orthodontics. Int J Adult Orthodon Orthognath Surg 2002. [Google Scholar]
- KJ Lee, E Joo, KD Kim. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop 2009. [Google Scholar]
- HS Park. An anatomical study using CT Images for the implantation of micro-implants. Korean J Orthod 2002. [Google Scholar]
- HS Park, SH Jeong, OW Kwon. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop 2006. [Google Scholar]
- C Chang, SSY Liu, WE Roberts. Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva. Angle Orthod 2015. [Google Scholar]
- M Motoyoshi, M Hirabayashi, M Uemura, N Shimizu. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res 2006. [Google Scholar]
- S Baumgaertel. Pre-drilling of the implant site - is it necessary for orthodontic mini-implants?. Am J Orthod Dentofacial Orthop 2010. [Google Scholar]
- S Kuroda, K Yamada, T Deguchi, T Hashimoto, HM Kyung, T Takano-Yamamoto. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop 2007. [Google Scholar]
- K Asscherickx, BV Vannet, H Wehrbein, MM Sabzevar. Success rate of miniscrews relative to their position to adjacent roots. Eur J Orthod 2008. [Google Scholar]
- YH Chen, HH Chang, YJ Chen, D Lee, HH Chiang, CCJ Yao. Root contact during insertion of miniscrews for orthodontic anchorage increases the failure rate: an animal study. Clin Oral Implants Res 2008. [Google Scholar]
- LC Hernandez, G Montoto, M Puente Rodríguez, L Galbán, V Martínez. 'Bone map' for a safe placement of miniscrews generated by computed tomography. Clin Oral Implants Res 2008. [Google Scholar]
- C Monnerat, L Restle, J N Mucha. Tomographic mapping of mandibular interradicular spaces for placement of orthodontic mini-implants. Am J Orthod Dentofacial Orthop 2009. [Google Scholar]
- SH Kim, HG Yoon, YS Choi, EH Hwang, YA Kook, G Nelson. Evaluation of interdental space of the maxillary posterior area for orthodontic mini-implants with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009. [Google Scholar]
- S Baumgaertel, MG Hans. Assessment of infrazygomatic bone depth for mini-screw insertion. Clin Oral Implants Res 2009. [Google Scholar]
- BT Brettin, NM Grosland, F Qian, KA Southard, TD Stuntz, TA Morgan. Bicortical vs monocortical orthodontic skeletal anchorage. Am J Orthod Dentofacial Orthop 2008. [Google Scholar]
- S Baumgaertel, MR Razavi, MG Hans. Mini-implant anchorage for the orthodontic practitioner. Am J Orthod Dentofacial Orthop 2008. [Google Scholar]
- B Wilmes, C Rademacher, G Olthoff, D Drescher. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop 2006. [Google Scholar]
- B Wilmes, D Drescher. Impact of bone quality, implant type, and implantation site preparation on insertion torques of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Surg 2011. [Google Scholar]
- HS Park. Clinical study on success rate of microscrew implant for orthodontic anchorage. Korea J Orthod 2003. [Google Scholar]
- M Umemori, J Sugawara, H Mitani, H Nagasaka, H Kawamura. Skeletal anchorage system for open bite correction. Am J Orthod Dentofacial Orthop 1998. [Google Scholar]
- CH Paik, YJ Woo, R Boyd. Treatment of an adult patient with vertical maxillary excess using miniscrew fixation. J Clin Orthod 2003. [Google Scholar]
- R Foot, O Dalci, C Gonzales, NE Tarraf, MA Darendeliler. The short-term skeleto-dental effects of a new spring for the intrusion of maxillary posterior teeth in open bite patients. Prog Orthod 2014. [Google Scholar] [Crossref]
- FK Byloff, MA Darendeliler. Distal molar movement using the pendulum appliance. Part 1: Clinical and radiological evaluation. Angle Orthod 1997. [Google Scholar]
- FK Byloff, MA Darendeliler, E Clar, A Darendeliler. Distal molar movement using the pendulum appliance. Part 2: The effects of maxillary molar root uprighting bends. Angle Orthod 1997. [Google Scholar]
- A Caprioglio, A Cafagna, M Fontana, M Cozzani. Comparative evaluation of molar distalization therapy using pendulum and distal screw appliances. Korean J Orthod 2015. [Google Scholar]
- C Sar, A Arman-Ozcirpici, S Uckan, A C Yazici. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
- M Nienkemper, B Wilmes, A Pauls, D Drescher. Maxillary protraction using a hybrid hyrax-facemask combination. Prog Orthod 2013. [Google Scholar] [Crossref]
- B Wilmes, B Ludwig, V Katyal, M Nienkemper, A Rein, D Drescher. The Hybrid Hyrax Distalizer, a new all-in-one appliance for rapid palatal expansion, early class III treatment and upper molar distalization. J Orthod 2014. [Google Scholar]
- A Buchter, D Wiechmann, S Koerdt, HP Wiesmann, J Piffko, U Meyer. Load-related implant reaction of mini-implant used for orthodontic anchorage. Clin Oral Implants Res 2005. [Google Scholar]
- A Costa, M Raffaini, B Melsen. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthod Orthognath Surg 1998. [Google Scholar]
- HS Park, SM Bae, HM Kyung. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod 2001. [Google Scholar]
- WE Roberts, KJ Marshall, PG Mozsary. Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod 1990. [Google Scholar]
- YC Hwang, HS Hwang. Surgical repair of root perforation caused by an orthodontic miniscrew implant. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
- H Liu, D Liu, G Wang. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am J Orthod Dentofacial Orthop 2010. [Google Scholar]
- EY Suzuki, B Suzuki. Accuracy of miniscrew implant placement with a 3-dimensional surgical guide. J Oral Maxillofac Surg 2008. [Google Scholar]
- S Kang, SJ Lee, SJ Ahn. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop 2007. [Google Scholar]
- M Alves, C Baratieri, C T Mattos. Root repair after contact with mini-implants: systematic review of the literature. Eur J Orthod 2013. [Google Scholar]
- CE Brisceno, PE Rossouw, R Carrillo, R Carrillo, R Spears, PH Buschang. Healing of the roots and surrounding structures after intentional damage with miniscrew implants. Am J Orthod Dentofacial Orthop 2009. [Google Scholar]
- H Kim, TW Kim. Histologic evaluation of root-surface healing after root contact or approximation during placement of mini-implants. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
- X Jia, X Chen, X Huang. Influence of orthodontic mini-implant penetration of the maxillary sinus in the infrazygomatic crest region. Am J Orthod Dentofacial Orthop 2018. [Google Scholar]
- M Desai, A Jain, N Sumra. Surgical management of fractured orthodontic mini-implant - A case report. J Clin Diagn Res 2015. [Google Scholar]
- S E Barros, G Janson, K Chiqueto. Effect of mini- implant diameter on fracture risk and self-drilling efficacy. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
- R Ahluwalia, A Kaul, G Singh. Microimplants fracture: prevention is better than cure. J Ind Orthod Soc 2012. [Google Scholar]
- BH Choi, J Li, HS Kim, CY Ko, SM Jeong, F Xuan. Ingestion of orthodontic anchorage screws: an experimental study in dogs. Am J Orthod Dentofacial Orthop 2007. [Google Scholar]
- J Sugawara, N Nishimura. Minibone plates: the skeletal anchorage system. Semin Orthod 2005. [Google Scholar]
- B K Cha, N K Lee, D S Choi. Maxillary protraction treatment of skeletal Class III children using miniplate anchorage. Korean J Orthod 2007. [Google Scholar]
- D Kaya, I Kocadereli, B Kan, F Tasar. Effectiveness of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions: a pilot study. Angle Orthod 2011. [Google Scholar]
- D Garib, M Yatabe, RAS Faco. Bone-anchored maxillary protraction in a patient with complete cleft lip and palate: a case report. Am J Orthod Dentofacial Orthop 2018. [Google Scholar]
- Introduction
- Materials Used for Implants
- Understanding Implant Sites for TADS
- Maxillary buccal alveolar bone
- Maxillary palatal alveolar bone
- Midpalatal suture
- Mandibular buccal alveolar bone
- Buccal shelf area
- Retromolar area
- Factors Affecting Implant Site Selection
- Technique of Miniscrew Placement
- Loading of Implant
- Clinical Application of TADS
- Open bite treatment
- Class II treatment and molar distalization
- Class III malocclusion
- Class III growth modification
- Intra-arch mechanics
- Advantages and Limiting Factors of Miniscrews and Miniplates for Orthodontic Treatment Miniscrews
- Conclusion
- Source of Funding
- Conflict of Interest
