- Visibility 128 Views
- Downloads 10 Downloads
- DOI 10.18231/j.jdp.2024.028
-
CrossMark
- Citation
Assessment of dental anxiety and dental fear among adult patients visiting to dental hospital in derabassi district: A survey based research
- Author Details:
-
Tulica Mittal
-
Navneet Kaur *
-
Gurpreet Kaur
Introduction
Anxiety is a negative emotional state of an inner disorder and an expectation of future danger accompanied by nervous behavior like biting nails or clenching and grinding teeth. Among various kinds of fear and phobia, dental anxiety is the most common among dental adult patients. The etiology of dental anxiety is not fully clear and is a multi-dimensional phenomenon. Anxious patients require extra time, are more challenging to manage, and present with behavioral problems that can cause stressful experiences for patients and dental surgeons. Research shows that many dentists are also stressed when treating petrified dental patients. Therefore, it is foremost to assess and evaluate one's dental anxiety levels for better management and a proper treatment plan.
According to oxford medicine online; “Anxiety refers to multiple mental and physiological phenomena, including a person's conscious state of worry over a future unwanted event, or fear of an actual situation. Anxiety and fear are closely related. Some scholars view anxiety as a uniquely human emotion and fear as common to non-human species. Another distinction often made between fear and anxiety is that fear is an adaptive response to realistic threat, whereas anxiety as a diffuse emotion, sometimes an unreasonable or excessive reaction to current or future perceived threat”.
The concept of anxiety has several possible meanings and may thus give rise to uncertainty and ambiguity.[1] All anxiety disorders share elements of fear and apprehensiveness, where the former is an emotional response to a real or perceived warning while the latter concerns expectations of a future peril. Anxiety is a common disorder with a lifetime prevalence of approximately 30%.[2] About one in two individuals diagnosed with anxiety disorders also meet the criteria for a depressive disorder[3] as a consequence, anxiety in dentistry has two clinical implications in routine clinical practice: (A) the high prevalence of anxiety disorders and depression in the general population, which may make people anxious during dental care as a result of trait anxiety; (B) a high prevalence of specific dental anxiety (DA and phobia (raising only the context of dental care which has been estimated to affect 10% to 30% of population depending on sample selection (i.e., general population or patients scheduled for intervention) ethnic and socio-cultural variables. [4] In 1984 Dr. Ulf Berggren studied the association between dental fear and avoidance behavior. [5] In conclusion, the author proposed the theory of a vicious cycle where dental fear would lead to dental care avoidance behavior resulting in neglect of the stomatognathic system over time, poorer oral health, and thus the need for more invasive procedures that subsequently increase the level of dental anxiety ([Figure 1]).
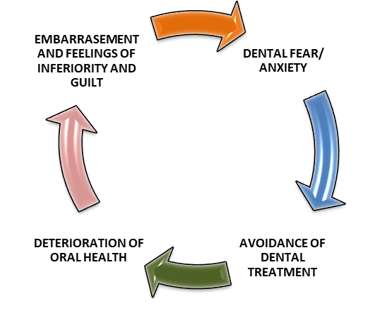
The self-perpetuating model has been assessed in whole or partially by several authors.[6], [7] De Jongh et al. tested the hypothesis that dental treatment avoidance and the fear of negative evaluation are mediated by the deterioration of oral health. [6] Besides supporting the assumptions, avoidance behavior over time is associated with poorer oral health. The author suggested that less dental health status was significantly associated with embarrassment related to dentition and negative social consequences. Alternative explanations for the avoidance behavior were described by DE Jongh et al.[6] and resembled what was previously proposed by Berggren[5] and Abrahamsson et al.[8] an exaggerated negative appraisal of the patient's oral status as a trigger to missing appointments where the possibility of meeting endodontic treatment, extractions, and deep fillings would result in more uncomfortable and painful sessions.
Dental anxiety arises due to multiple factors, such as previous childhood experience, learning from anxious family and friends, individual personality characteristics, lack of information, exposure to scary dentist's portraits in the media, and the vulnerability of lying ones once back in a dental chair. [9] Sensory stimuli like the sounds of drilling and screaming, the smell of certain dental materials or body fluids (blood or pus), and the sights of needle and air turbine drills provoke anxiety and are related to a patient's behaviors as the sense of conduct, experiences, and overall mental health. Oosterink et al. 2009 discussed how dental phobia is usually related to 10 other common fears or phobias such as injections flying, snakes, closed spaces, and others.
Numerous measures are being refined for identifying dentally anxious patients and assessing the level of dental fear. These range from single dental anxiety questions to multiple-item scales, like Corah’s Dental Anxiety Scale, DAS (Corah 1969),[10] Kleinknecht’s Dental Fear Survey DFS (Kleinknecht et al. 1973),[11] and modified dental anxiety scale, MDAS (Humphri et al).[12] The anxiety questions and scales measures different aspects of dental fear and is recommended to be used for various purposes.
Corah’s DAS is an accepted tool to measure anxiety among adults. The DAS is a 4-item questionnaire that asks respondents to indicate their emotional reaction: anticipating dental appointment, in the waiting room, anticipating drilling, and anticipating scaling. Each question has five response alternatives. In earlier research, DAS is correlated highly with observed and reported dental anxiety. Measuring dental fear with the DAS, scores 13 and higher are supposed to indicate dental anxiety, and scores 15 and higher phobic level of dental fear. The DAS has certain limitations and focuses on only the cognitive dimension of anxiety to a limited validity. The DAS was modified to MDAS by introducing questions concerning local anesthesia and simplifying answers by standardizing the answer categories. MDAS has five questions with five response alternatives ranging from; "not anxious" (score 1) to “extremely anxious” (score 5). MDAS is a reliable and valid measure of dental anxiety. The MDAS is habituated analogously to DAS for screening dental anxiety and brief measures in epidemiological studies. Both are the most popular tool for the assessment of dental fear
Phobic dental patients always avoid dental administration, seek emergency dental care, postpone their dental visits, and have poor oral health-related quality of life. Identifying dental anxiety among dental patients is crucial for management and decision-making regarding treatment. Since there is sparse information available in the literature on the impact of dental anxiety among adult patients, the study was conducted to assess the level of anxiety toward dental treatments among dental patients who visited a dental hospital.
Materials and Methods
A cross-sectional survey was used to assess the dental anxiety levels of patients in the Derabassi district. More specifically, the Study was conducted at National Dental College and Hospital Derabassi, Punjab, India. Eligible participants of both genders (Male and Female) with the age group of 20-60 years who seeks dental treatment and consultation were included in the study. Participants who were willing to participate as a volunteer were also included in the study. Dental practitioners (dental students, interns, postgraduate dental students), pregnant women, and patients with mental disabilities or any neurological disorder or malignancy were excluded from the study.
Convenience sampling was done, and data was collected from 467 participants coming to the dental OPD of National Dental College and Hospital Derabassi. The questionnaire was designed and structured in English, Hindi, and Punjabi dialects to improve validity and consisted of 24 questions divided into three parts. The first part of the questionnaire was used to obtain information on the socio-demographic details (age, gender, occupation, and educational status) of the participants. The second part of the questionnaire consists of 9 questions providing detailed information on previous dental visits and treatments, medical history, and oral hygiene status of the patients.
The third part was a modified dental anxiety scale (MDAS) which is a self-reported measure of the Likert scale with values between 1-5 (1= anxious - 5= extremely anxious) was used to assess the levels of dental anxiety about an upcoming dental visit, the dentist’s waiting room, having a tooth drilled, scaling and polishing of the teeth, local anesthetic injection and oral surgery procedure include surgical extractions, replacement of teeth and orthodontic treatment. The total score of MDAS ranged from 5 to 25. The patient's score of 0-10 was considered slightly/non anxious. Scores from 11 to 14 were fairly anxious and scores from 15 to 25 were very anxious and dental phobic.
The questionnaire proforma was handed to the respective dental patients in the outpatient department of dental hospital Derabassi during the routine visit to the dental patients.
Statistical analysis
The data for the present study was entered into Microsoft Excel 2007 and analyzed using the SPSS statistical software 23.0 Version. The descriptive statistics included mean and standard deviation. The level of significance for the present study was fixed at 5%. The inter-response comparison was done using the Chi-square test and multivariate logistic regression analysis was used to find an association between the dependent and independent variables.
Result
Out of 500 participants, 467 participants responded positively by participating in this study. In this way, the response rate was 93.4%. The rest of the participants didn’t complete the questionnaire, and incomplete data were excluded from the survey. Some participants refused to participate in the study or because of lack of time.
Socio-demographic characteristics
The demographic details of the study participants are presented in [Table 1], among a total of 467 participants, 225 (48.1%) were males and 242 (51.8%) were females. The majority of participants (30.6%) were aged between 31-40 years followed by the 20-30 years age group (26.9%), while the age groups of 41-50 years comprise (22%) and the ˃50 years and above represent (20.3%) of the sample. Most of the participants were employed (65.1%), whereas only 34.9% were unemployed. The educational levels of the majority of the participants were 46.6% with graduation, and 22.2% had postgraduate/Ph.D. and school degrees.
|
Parameters |
Variables |
N |
Percentage |
|
Age Groups |
20-30 years |
126 |
26.98% |
|
31-40 years |
143 |
30.62% |
|
|
41-50 years |
103 |
22.05% |
|
|
>50 years |
95 |
20.35% |
|
|
|
|
|
|
|
Gender |
Male |
225 |
48.19% |
|
Female |
242 |
51.81% |
|
|
|
|
|
|
|
Occupation |
Employed |
304 |
65.10% |
|
Unemployed |
163 |
34.90% |
|
|
|
|
|
|
|
Educational Status |
Primary education (5th class) |
39 |
8.35% |
|
Secondary education (10th /12th class) |
106 |
22.70% |
|
|
Graduate |
218 |
46.68% |
|
|
Postgraduate/ PhD |
104 |
22.27% |
Study participants’ attitudes toward oral health behavior ([Table 2])
More than half of the participants in the sample were regular visitors to the dentist (67.6%), while, 32.3% of the participants were irregular visitors to the dentist and only 23.7% routinely visited the dentists. A maximum number of participants (17.3%) visited to dentists with a chief complaint of painful tooth and extraction while 15.8% visited because of dental caries and bleeding gums. 58.6% of participants agreed that they visited the dentist for dental treatment whereas 41.3% of participants were not visited the dentist and did not undergo any dental treatment. One-fourth (35.3%) of participants visited the dentist once a year while 13.7% of participants visited dentists on a need basis only. The majority of participants (53.9%) agreed that they used to do tooth brushing once a day while only 27.8% of participants brushed their teeth twice a day. Regarding the time of tooth brushing, the majority of participants (80.5%) did tooth brushing before meals and 54.8% of participants take one minute for tooth brushing. Half of the participants (49.6%) agreed upon using various types of interdental cleaning aids (interdental brush, dental floss, or mouthwash).
|
Did you ever visit the dentist before? |
Yes |
316 |
67.67% |
|
No |
151 |
32.33% |
|
|
|
|
|
|
|
Why did you visit the dentist? |
Painful teeth |
76 |
16.27% |
|
Tooth extraction |
81 |
17.34% |
|
|
Routine visit |
111 |
23.77% |
|
|
Dental caries |
74 |
15.85% |
|
|
Bleeding gums |
69 |
14.78% |
|
|
Misaligned/ crowded teeth |
56 |
11.99% |
|
|
|
|
|
|
|
Did you undergo any dental treatment? |
Yes |
274 |
58.67% |
|
No |
193 |
41.33 |
|
|
|
|
|
|
|
How often do you visit the dentist? |
Once a year |
165 |
35.33% |
|
Twice a year |
87 |
18.63% |
|
|
On need basis only |
64 |
13.70% |
|
|
Never visited |
151 |
32.34% |
|
|
|
|
|
|
|
Do you suffer from any medical condition? |
Yes |
152 |
32.55% |
|
No |
315 |
67.45% |
|
|
|
|
|
|
|
How many times a day do you brush your teeth? |
Once daily |
252 |
53.96% |
|
Twice daily |
130 |
27.84% |
|
|
After every meal |
85 |
18.20% |
|
|
Greater than 2 times |
|
0 |
|
|
|
|
|
|
|
How much time do you take for each brushing? |
1 minute |
256 |
54.82% |
|
2 minute |
149 |
31.90% |
|
|
More than 2 minute |
62 |
13.28% |
|
|
|
|
|
|
|
Time of brushing |
Before Meals |
376 |
80.51% |
|
After Meals |
91 |
19.49% |
|
|
|
|
|
|
|
Do you use any other oral hygiene aid (interdental brush, dental floss, mouth wash) |
Yes |
232 |
49.68% |
|
No |
235 |
50.32% |
Response of participants to the modified dental anxiety scale (MDAS)
Overall responses to the anxiety scale questionnaire varied with different parameters ([Table 3]). In the first question in Modified Dental Anxiety Scale (MDAS), asking the patient about his/her anxiety level when anticipating a treatment for the next day, the average participants (31.9%) were slightly anxious and 23.9% were fairly anxious about visiting the dentist. Regarding the anxiety level, while sitting in the dentist’s waiting room, the average participants (28%) were fairly anxious whereas 19.4% were very anxious and 15.8% were extremely anxious sitting in the Waiting Room. Anxiety level was increased to fairly anxious; when the participants/dental patients (25.6%) were asked about getting their teeth drilled. However, the mean percentage of dental anxiety levels dropped to slightly anxious (5.9%) for the question about extraction or any surgical procedure, which were the least anxiety levels in the respondents compared to the other parameter of dental situations and procedures. The anxiety level was increased dramatically in the parameter of a local anesthetic injection in the gum with the mean percentage of the participants (10%) being fairly anxious. The anxiety level was increased furthermore with the tooth extraction and dental surgical procedure. Results showed that the average of the participants in the sample (51.1%) was fair to extremely anxious about having their tooth extracted or having dental surgical treatment. Regarding the tooth to be replaced, 28.6% of participants were fairly anxious whereas 22.2% of participants were fairly anxious when they were about to undergo an Orthodontic Treatment. The inter-response variation was found to be statistically significant for all variables when analyzed using the Chi-square test at p-value ˂ 0.001
|
|
Not Anxious |
Slight Anxious |
Fairly Anxious |
Very Anxious |
Extremely Anxious |
P value |
|
If You Went To Your Dentist For Treatment Tomorrow, How Would You Feel? |
70 |
149 |
112 |
74 |
62 |
0.001 (Sig) |
|
14.99% |
31.91% |
23.98% |
15.84% |
13.28% |
||
|
If You Were Sitting In The Waiting Room (Waiting For Treatment), How Would You Feel? |
72 |
99 |
131 |
91 |
74 |
0.001 (Sig) |
|
15.42% |
21.19% |
28.05% |
19.49% |
15.85% |
||
|
If You Were About To Have A Tooth Drilled/Restoration, How Would You Feel? |
62 |
72 |
120 |
117 |
96 |
0.001 (Sig) |
|
13.27% |
15.42% |
25.69% |
25.06% |
20.56% |
||
|
If You Were About To Have A Local Anesthetic Injection In Your Gums, How Would You Feel? |
55 |
47 |
90 |
113 |
162 |
0.001 (Sig) |
|
11.77% |
10.06% |
19.27% |
24.20% |
34.70% |
||
|
If Your Third Molar Or Any Other Teeth Were About To Be Removed Through Any Surgical Procedure/ Extraction How You Would Feel? |
44 |
28 |
58 |
98 |
239 |
0.001 (Sig) |
|
9.43% |
5.99% |
12.42% |
20.98% |
51.18% |
||
|
If You Were About To Have Your Teeth Scaled And Polished, How Would You Feel? |
63 |
75 |
82 |
112 |
135 |
0.001 (Sig) |
|
13.49% |
16.06% |
17.56% |
23.98% |
28.91% |
||
|
If You Were About To Have Your Tooth Replaced, How Would You Feel? |
97 |
81 |
134 |
96 |
59 |
0.001 (Sig) |
|
20.78% |
17.34% |
28.69% |
20.56% |
12.63% |
||
|
If You Were About To Undergo An Orthodontic Treatment, How Would You Feel? |
151 |
102 |
104 |
65 |
45 |
0.001 (Sig) |
|
32.33% |
21.84% |
22.27% |
13.92% |
9.64% |
Mean anxiety score for the modified dental anxiety scale
The mean anxiety scores were assessed for each question for the Modified Dental Anxiety Scale (MDAS) as shown in [Table 4]. The highest anxiety mean scores (3.98±1.31) were recorded for third molar Extraction or surgical procedures followed by injection of Local Anesthetics with a mean anxiety score of 3.6±1.35 followed by scaling and polishing mean anxiety score of 3.39±1.40 followed by tooth drilled/restoration with a mean anxiety score was 3.24±1.30. However, the least mean anxiety scores recorded for the replaced tooth as well as orthodontic treatment were 2.87±1.30 and 2.47±1.32 respectively.
|
Anxiety Question |
Mean |
SD |
|
1. If You Went To Your Dentist For Treatment Tomorrow, How Would You Feel? |
2.8 |
1.25 |
|
2. If You Were Sitting In The Waiting Room (Waiting For Treatment), How Would You Feel? |
2.99 |
1.29 |
|
3. If You Were About To Have A Tooth Drilled/Restoration, How Would You Feel? |
3.24 |
1.30 |
|
4. If You Were About To Have A Local Anesthetic Injection In Your Gums, How Would You Feel? |
3.6 |
1.35 |
|
5. If Your Third Molar Or Any Other Teeth Were About To Be Removed Through Any Surgical Procedure/ Extraction How You Would Feel? |
3.98 |
1.31 |
|
6. If You Were About To Have Your Teeth Scaled And Polished, How Would You Feel? |
3.39 |
1.40 |
|
7. If You Were About To Have Your Tooth Replaced, How Would You Feel? |
2.87 |
1.30 |
|
8. If You Were About To Undergo An Orthodontic Treatment, How Would You Feel? |
2.47 |
1.32 |
|
Total Score |
25.34 |
8.12 |
Logistic regression analysis for the association between socio-demographic variables and dental anxiety
Based on the logistic regression, analysis concerning dental anxiety in [Table 5] shows that there was a significantly high dental anxiety average score among females as compared to males (adjusted OR 1.935 with 95% CI of 1.57-2.51). The result of the study showed that Patients with no previous dental visit were more likely to suffer from dental anxiety as compared to their counterparts (adjusted OR 2.235 with 95% CI of 1.26-3.10). Those subjects having the primary and secondary level of education were more likely to suffer from dental anxiety as compared to their having graduation and post-graduation education level (adjusted OR 1.58 with 95% CI of 0.76-3.2). The study revealed that there were no significant differences in the averages of dental anxiety scores comparable in different classes of age and occupations.
|
|
P value |
Odd Ratio |
95.0% C.I. for EXP(B) |
|
|
Age Groups |
Lower |
Upper |
||
|
20-30 years |
0.090 (Non-Sig) |
0.543 |
.268 |
1.100 |
|
31-40 years |
0.743 (Non-Sig) |
0.885 |
.427 |
1.835 |
|
41-50 years |
0.353 (Non-Sig) |
0.703 |
.334 |
1.480 |
|
>50 years |
- |
1.000(Constant) |
- |
- |
|
Gender |
|
|
|
|
|
Female |
0.001 (Sig) |
1.935 |
1.578 |
2.514 |
|
Male |
- |
1.000(Constant) |
|
|
|
Occupation |
|
|
|
|
|
Employed |
1.000 (Non-Sig) |
0.234 |
0.127 |
0.345 |
|
Unemployed |
- |
1.000(Constant) |
|
|
|
Education |
|
|
|
|
|
Primary education (5th class) |
0.031 (Sig) |
1.703 |
.283 |
1.745 |
|
Secondary education (10th /12th class) |
0.042 (Sig) |
1.581 |
.763 |
3.276 |
|
Graduate |
0.045 (Sig) |
1.404 |
.793 |
2.486 |
|
Post Graduate |
- |
1.000(Constant) |
|
|
|
Previous Dental Visit |
|
|
|
|
|
No |
0.043 (Sig) |
2.235 |
1.268 |
3.100 |
|
Yes |
- |
1.000(Constant) |
|
|
Discussion
Visiting dental practitioners may cause different levels of anxiety for many individuals. Most patients learn to manage their anxiety levels; some improve their emotions and behaviors through routine dental assistance, and a minority still exhibit high anxiety. [13] This study targeted patients who suffer from high dental anxiety, are at risk of avoiding dental care, and may subsequently suffer from poor oral health. Patients who delay or avoid routine dental care need emergency dental treatment involving invasive and surgical procedures that could aggravate their anxiety levels. Despite the advancement in modern dentistry, anxiety about dental treatments remains prevalent. Dental anxiety affects individuals and their life, ranging from their overall well-being and satisfaction to self-esteem and daily masticatory function.[14] Healthcare professionals should attempt to identify these individuals to provide better care and improve access to dental care.
The study was conducted to assess dental anxiety levels among patients who visited the dental hospital in the Derabassi district. The mean total dental anxiety score was 25.34 (SD ± 8.12), which is higher than the anxiety levels reported from studies in India (Acharya, 2008),[15] Saudi Arabia (Fayad et al., 2017)[16] with the mean dental anxiety score was 11.39 (SD ± 2.7), Spain (Coolige et al., 2010)[17] with overall dental anxiety mean score was 11.8 (SD ± 5.1), Iran (Saatchi et al., 2015)[18] with the mean score was 12.34 (SD ± 4.74), UAE college populations (Hawamdeh and Awad, 2013)[19] with the mean score was 11.52 (SD ± 4.88). The present study showed a higher mean value compared to previously reported studies. All the patients included in the study underwent surgical procedures or extractions which were more invasive than conventional dental check-ups or restorative work and scored high DA values. Based on the severity of dental anxiety in each parameter of MDAS, dental surgical procedures and extractions scored the highest mean anxiety score with a mean of 3.98 (SD ± 1.31), which was similar to the findings in Saudi Arabia (Gaffar et al., 2014),[20] Turkey (Erten et al., 2006)[21] and in China (Yuan et al., 2008).[22]
The study showed a significant difference (p=0.001) in dental anxiety levels between males (mean total anxiety score 1.000) and females (mean total anxiety score 1.935), a possible explanation of females being more emotional than males. This result is in agreement with the studies by Erten et al. (2006),[21] Coolidge et al. (2008),[17] Saatchi et al. (2015),[18] and Fayad et al. (2017)[16] However, the majority of the studies revealed similar anxiety results between males and females (Al-Madi & Hoda 2002).[23] The observed difference between males and females might be due to a real difference in the anxiety levels between genders, a greater readiness among females to acknowledge feelings of anxiety, and both factors acting in combination. The results from this study showed that there was no relationship between age and dental anxiety score. The finding is similar to the findings of Erten et al. (2006)21 and Saatchi et al. (2015)[18] who reported that dental fear and anxiety were not affected by age. Contrary to the findings of Acharya (2008)[15] and Fayad et al. (2017) [16] reported an inverse relationship between age and dental anxiety score.
Regarding education, the results of the present study showed that dental anxiety score was higher in patients with primary and secondary levels of education compared to the graduation and post-graduation levels of education. The results agreed with the study by Erten et al. (2006) [21] and showed that education level does not affect dental anxiety, the results did not agree with the study by Akeel et al. (2000) that outlined, patients with a higher level of education were highly anxious.
The study revealed a significant difference in dental anxiety scores in patients having no past dental visits. Studies were done by Acharya (2008)[15] and Saatchi et al. (2015)18 reported that patients with past dental visits showed less anxiety than patients with no past dental visits. The main reason for irregular dental visits was due to lack of time and no need for treatment rather than due to dental anxiety Taani (2001).[24] A study conducted by Malvania et al. (2011)[25] reported that dental anxiety was not associated with previous dental visits.There are several notions as to how dental anxiety may arise. In reality, multiple factors combine to initiate and maintain feelings of apprehension. Some patients are afraid of the stimuli involved with dental treatment and revealed the highest score in MDAS parameter in the study by Gaffar (2014),[20] which affects the dental treatment plan and the patient-dentist relationship. Anxiety and fear levels are assessed with an empathic approach to the patient and dentist's behavior beforehand. The use of sedation and hypnosis is considered the first step of dental care and implements the wise use of anxiolytic drugs to get full conscious sedation while keeping general anesthesia for selected cases only. The European recommendations about conscious sedation stated it was the safest and simplest way of managing the patient and improving safety through emergency prevention rather than being a cause of adverse events.
Such studies inevitably encounter some limitations and meticulous care taken to exclude patients with psychological disorders, which may influence the assessment of anxiety. Some patients got eliminated from the study based on their responses. Another accepted limitation is cross-sectional design of the survey does not provide information on causality. Also, a self-administered questionnaire could be biased, as there are chances that patients may over or underestimate their responses. Further assessment and analysis of dental anxiety levels associated with dental treatment may provide additional information for better patient management and a proper treatment plan for patients suffering from dental anxiety. There is a need for an appropriate scale that includes the patient's evaluation and the doctor's observation to analyze dental anxiety.
Conclusion
Within the study limitations, it can be concluded that the prevalence of dental anxiety was moderate among the study subjects. Amongst the various socio-demographic factors, gender and educational level were significantly associated with dental anxiety. On the other hand, there is no significant difference in dental anxiety levels based on age and occupation.
Further studies are needed to address dental anxiety levels in different populations, which will help dental care providers to manage patients in a better way. More information should emerge in this field since specialties in dentistry are becoming more available to the public. The development of dental anxiety could be prevented with pain control, behavior management, and consideration of the patient. The inclusion of behavioral sciences in dental education and the integration of ethical considerations in the academic dental curriculum could help improve the situation.
Source of Funding
None.
Conflict of Interest
None.
References
- E Facco, D Lucangeli, P Tressoldi. On the science of consciousness: epistemological reflections and clinical implications. Explore 2017. [Google Scholar]
- R C Kessler, P Berglund, O Demler, R Jin, KR Merikangas, EE Walters. Lifetime prevalence and age-of-onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005. [Google Scholar]
- NM Batelaan, J Spijker, R De Graaf, P Cuijpers. Mixed anxiety depression should not be included in DSM-5. J Nerv Ment Dis 2012. [Google Scholar]
- E Facco, E Gumirato, G Humphris, E Stellini, C Bacci, S Sivolella. Modified Dental Anxiety Scale: validation of the Italian version. Minerva Stomatol 2015. [Google Scholar]
- U Berggren, G Meynert. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc 1984. [Google Scholar]
- A De Jongh, M Schuties, IHA Aartman. A test of Berggrens’ model of dental fear and anxiety. Eur J Oral Sci 2011. [Google Scholar]
- W Sohn, AI Ismail. Regular dental visits and dental anxiety in an adult dentate population. J Am Dent Assoc 2005. [Google Scholar]
- K Henning Abrahamsson, U Berggren, M Hakeberg, SG Cerlsson. Phobic avoidance and regular dental care in fearful dental patients: a comparative study. Acta Odontol Scand 2001. [Google Scholar]
- DP Appukuttan. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin Cosmet Investing Dent 2016. [Google Scholar] [Crossref]
- NL Corah. Development of a dental anxiety scale. J Dent Res 1969. [Google Scholar] [Crossref]
- RA Kleinknecht, RK Klepac, LD Alexander. Origins and characteristics of fear of dentistry. J Am Dent Assoc 1973. [Google Scholar]
- GM Humphris, T Morrison, SJ Lindsay. The Modified Dental Anxiety Scale: validation and United Kingdom norms. Community Dent Health 1995. [Google Scholar]
- SH Addicks, DW Mcneil, CL Randall, A Goddard, LM Romito, C Sirbu. Dental care-related fear and anxiety: distress tolerance as a possible mechanism. JDR Clin Transl Res 2017. [Google Scholar]
- NP Crofts-Barnes, E Brough, KE Wilson, AJ Beddis, NM Girdler. Anxiety and quality of life in phobic dental patients. J Dent Res 2010. [Google Scholar]
- S Acharya. Factors affecting dental anxiety and beliefs in an Indian population. J Oral Rehabil 2008. [Google Scholar] [Crossref]
- MI Fayad, A Elbieh, MN Baig, SA Alruwaili. Prevalence of Dental Anxiety among Dental Patients in Saudi Arabia. J Int Soc Prev Community Den 2017. [Google Scholar]
- T Coolidge, KN Arapostathis, D Emmanouil, N Dabarakis, A Patrikiou, N Economides. Psychometric properties of Greek versions of the Modified Corah Dental Anxiety Scale (MDAS) and the Dental Fear Survey (DFS). BMC Oral Health 2008. [Google Scholar] [Crossref]
- M Saatchi, M Abtahi, G Mohammadi, M Mirdamadi, ES Binandeh. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent Res J (Isfahan) 2015. [Google Scholar]
- S Hawamdeh, M Awad. Dental anxiety: Prevalence and associated factors. Eur J Gen Dent 2013. [Google Scholar]
- BO Gaffar, AS Alagl, AA Al-Ansari. The prevalence, causes, and relativity of dental anxiety in adult patients to irregular dental visits. Saudi Med J 2014. [Google Scholar]
- H Erten, ZZ Akarslan, E Bodrumlu. Dental fear and anxiety levels of patients attending a dental clinic. Quintessence Int 2006. [Google Scholar]
- S Yuan, R Freeman, S Lahti, F Lloyd-Williams, G Humphris. Some psychometric properties of the Chinese version of the Modified Dental Anxiety Scale with cross validation. Health Qual Life Outcomes 2008. [Google Scholar] [Crossref]
- EM Al-Madi, AL Hoda. Assesment of dental fear and anxiety among adolescent females in Riyadh Saudi Arabia. Saudi Dent J 2002. [Google Scholar]
- DSQ Taani. Dental fear among a young adult Saudian population. Int Dent J 2001. [Google Scholar]
- EA Malvania, CG Ajithkrishnan. Prevalence and socio-demographic correlates of dental anxiety among a group of adult patients attending a dental institution in Vadodara city. Indian J Dent Res 2011. [Google Scholar]
- Introduction
- Materials and Methods
- Result
- Socio-demographic characteristics
- Study participants’ attitudes toward oral health behavior ([Table 2])
- Response of participants to the modified dental anxiety scale (MDAS)
- Mean anxiety score for the modified dental anxiety scale
- Logistic regression analysis for the association between socio-demographic variables and dental anxiety
- Discussion
- Conclusion
- Source of Funding
- Conflict of Interest
