- Visibility 63 Views
- Downloads 16 Downloads
- DOI 10.18231/j.jdp.2024.033
-
CrossMark
- Citation
Decode telangiectatic granuloma- A case report
- Author Details:
-
Rabia Zarrin
-
Manisha
-
Supratik Roy
-
Annapurna Ahuja *
Introduction
A benign hyperplastic lesion known as an oral telangiectatic granuloma develops in the mouth as a result of trauma or long-term irritation.[1] Pyogenic granuloma, commonly known as telangiectatic granuloma, is a benign, hyperplastic, inflammatory, and rapidly developing lesion of the soft tissues. It may affect the skin, oral mucosa, gingiva, lips, tongue, and skin itself. It bleeds readily when provoked. [2]
The lesion is not clinically or histopathologically associated with any type of infection, such as pus development, hence the name "pyogenic granuloma" is misleading. In actuality, it is the result of a variety of stressors, including hormonal changes, certain medicines, traumatic injuries, and mild local irritation. It primarily affects young females in their second decade of life, maybe as a result of the vascular effects of female hormones. [3] It is considered non neoplastic in nature. Surgical excision was planned due to hinderance in mastication which could lead to bleeding & other complication such as relapse. [4], [5]
This entity has been referred to by a number of names, some of which reflect incorrect ideas about its etiopathogenesis: septic granuloma, hemangiomatous granuloma, lobular capillary hemangioma, Eruption capillary granuloma, benign pedunculated granuloma, pseudobotryomycosis, fibroangioma, croker and Hartzell disease, telangiectatic granuloma, benign pedunculated granuloma, pseudobotryomycosis and fibroangioma. [6], [7], [8] Its prevalence rate is between 6 and 10%, and it is more frequent in women. [9]
“Telangiectasia” is a more appropriate term, given its literal meaning in Greek of “distant dilated capillary vessel.” The Latin term “pyogenic” is considered a misnomer since it is often erroneously associated with an infectious origin. It develops as a response to the local trauma or chronic irritation creating a repair tissue (granulation) produced by the body as a defence mechanism. Instead of the usual distribution in globules, the staphylococci are primarily located on the surface. Yet, as seen by the term granuloma pyogenicum, authors are once again inclined to recognise the pathogenetic significance of staphylococci. [10], [11]
Cawson et al, due to presence of various blood vessels in oral pyogenic granuloma, suggested the term ‘Granuloma Telangiectacticum’. [12]
Angelopoulos AP suggested the term “hemangiomatous granuloma” that expressed histopathologically like hemangiomaand the inflammatory nature (granuloma) of oral pyogenic granuloma. [13]
Case Report
A swelling in the mandibular front tooth region of the jaw that had been present for two months was the main complaint of an 18-year-old female patient who was sent to the department of periodontology from the department of oral medicine and radiology at the Hazaribagh College of Dental Sciences & Hospital in Demotand, Jharkhand. The patient also reported slight increase in size of the growth along with no pain. There were no history of blood or pus discharge from the site. There was no contributory medical or drug history and no associated deleterious habits.
On intraoral examination it was seen as a tumour that was spherical in shape, was pedunculated. The lesion, which was roughly 10 mm in length and 8 mm in diameter, was found in the right para-midline region of the mandibular arch. The nature of the lesion ranged from soft to firm, and applying pressure caused it to blanch. The associated teeth were not mobile. The lesion was painless unless touched or applied pressure while brushing. The outer part of the lesion was pinkish red in colour.
Patient’s medical history was taken, and she reported no relevant history and her consent was also taken. On the day of surgery, she underwent some lab investigations. Blood examination like complete blood count, bleeding time & clotting time was investigated to prevent any complication during surgery.
During the surgical procedure, a local anaesthetic solution containing 2% lignocaine hydrochloride was injected into the surrounding tissues to perform an excisional biopsy. The tissue/tumour was excised with the help of no.15 scalpel. After being fixed in 10% formalin, the removed specimen was sent for histological examination to the department of oral pathology.
Patient was recalled after one week for re-evaluation of assessment of healing of that site which confirmed uneventful healing & patient was satisfied with this treatment modality.


Differential diagnosis
The differential diagnosis was capillary haemangioma, fibroma, and peripheral giant cell granuloma.
Histopathological examination
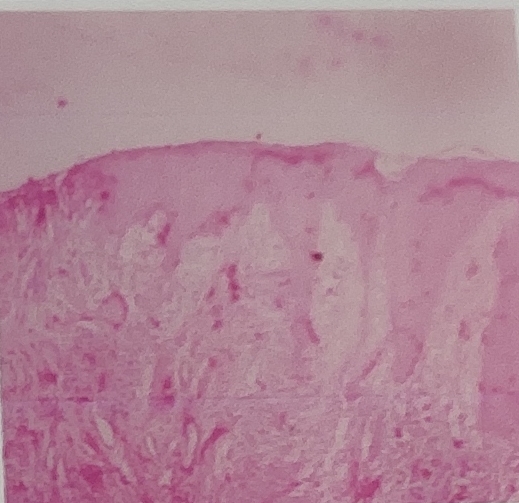
The provided H&E-stained section displays a stratified squamous epithelium that is parakeratinized, covering a highly cellular connective tissue that is characterized by the plump proliferation of endothelial cells, fibroblasts, and many budding capillaries. Chronic inflammatory cells within a matrix of collagen, predominantly plasma cells & lymphocytes are noted.
Histopathological diagnosis
Based on Clinico-Pathological connection, the overall findings are suggestive of Telangiectatic Granuloma (Capillary Phase/Vascular Phase).
Final diagnosis
Based on clinico-pathologic correlation, the lesion was diagnosed as Telangiectatic Granuloma.
Discussion
The most frequent way to describe a telangiectatic granuloma is as a pedunculated or sessile growth with a smooth or lobulated surface. Although lesions have also been seen on the palate, buccal mucosa, tongue, and lips, the gingiva is the most common intra-oral location of occurrence. Extraoral inflammation affects the mucous membranes of the nose and eyelids, as well as the skin of the neck, face, upper and lower limbs. The colour of the lesion can vary from red to pink depending on how mature it is, and the surface may become ulcerated. Depending on how advanced it is, the lesion's colour might range from red to pink, and its surface may develop ulcers. [14]
Local irritants or traumatic factors are associated to the development of this illness. [15] Oestrogen, progesterone, and testosterone [16] have vascular effects, which is why females are more commonly affected during puberty, pregnancy, and menopause. The primary course of treatment for Telangiectatic Granuloma is elimination of the etiological cause. This is followed by surgical excision, which can be carried out using either a traditional scalpel technique, electrocautery, cryotherapy, or other soft tissue lasers as diode CO2 laser, etc. [17] Although the treatment option for Telangiectatic Granuloma is surgical excision still the recurrence chance is 3% – 8.2%. [17]
Conclusion
The incidence of oral lesions still poses a diagnostic conundrum and a clinical mystery. Gingival growths can be challenging to categorize and distinguish based only on their clinical appearance and genesis. To establish a conclusive diagnosis, a gingival biopsy and subsequent histological evaluation are therefore essential. Prophylactic measures and careful management of the lesion are essential to reduce the likelihood of a recurrence.
Source of Funding
None.
Conflict of Interest
None.
References
- A Rathore, T Jadhav, A Kulloli, A Singh. Oral telangiectatic granuloma with an intrabony defect. J Indian Soc Periodontol 2015. [Google Scholar]
- F Shaikh, V Thorat, A Shaikh, S Muglikar, H Bhagwat. Treatment of Telangiectatic Granuloma by Electrocautery and Its Revie. Int J Sci Res 2022. [Google Scholar]
- H Jafarzadeh, M Sanatkhani, N Mohtasham. Oral pyogenic granuloma: a review. J Oral Sci 2006. [Google Scholar]
- K Mubeen, KR Vijayalakshmi, RP Abhishek. Oral pyogenic granuloma with mandible involvement: An unusual presentation. J Dent Oral Hyg 2011. [Google Scholar]
- A Vilmann, P Vilmann, H Vilmann. Pyogenic granuloma: evaluation of oral conditions. Br J Oral Maxillofac Surg 1986. [Google Scholar]
- JA Regezi, J Sciubba, RCK Jordan. . Oral Pathology: Clinical Pathologic Correlations 2016. [Google Scholar]
- LW Burket, MS Greenberg, M Glick. . Burket's oral medicine: diagnosis & treatment 2003. [Google Scholar]
- WG Shafer, MK Hine, BM Levy. Cysts and tumors of odontogenic origin. Textbook of Oral Pathology 1983. [Google Scholar]
- A Truschnegg, S Acham, B A Kiefer, N Jakse, A Beham. Epulis: a study of 92 cases with special emphasis on histopathological diagnosis and associated clinical data. Clin Oral Investig 2016. [Google Scholar]
- RV Subramanyam. Misnomers in oral pathology. Oral Dis 2010. [Google Scholar]
- NM Shah, V Shah, M H Shah, H Shrivastava. Recurrent telangiectatic granuloma in floor of the mouth (an unusual location). J Ahmedabad Dent CollHosp 2015. [Google Scholar]
- RA Cawson, WH Binnie, PM Speight, AW Barrett, JM Wright. . Lucas's pathology of tumors of the oral tissues 1998. [Google Scholar]
- AP Angelopoulos. Pyogenic granuloma of the oral cavity; statistical analysis of its clinical features. J Oral Surg 1971. [Google Scholar]
- SK Sachdeva. Extragingival pyogenic granuloma: an unusual clinical presentation. Journal of dentistry 2015. [Google Scholar]
- P Ghodke, R Hegde, S Lambe, W Ansari, S Muglikar. Management of Oral Telangiectatic Granuloma with 810 nm Diode Laser in a Medically Compromised Patient: A Case Report. Dentist 2019. [Google Scholar]
- BW Neville, DD Damm, CM Allen, JE Bouquot, BW Neville, DD Damm, CM Allen, JE Bouquot. Soft tissue tumors. Oral and Maxillofacial Pathology 2009. [Google Scholar]
- SR Dhande, B Jabade, S Muglikar, P Ghodke, A Doshi, B Harshad. Diode laser for excisional biopsy of combined gingival enlargement: a case report. The Dent 2021. [Google Scholar]
