- Visibility 1.4k Views
- Downloads 385 Downloads
- Permissions
- DOI 10.18231/j.jdp.2024.035
-
CrossMark
- Citation
3D printing – A paradigm shift in orthodontic appliances and patient care
- Author Details:
-
G Sreejith Kumar *
-
C Priya Dharshini
-
Prasanth Soni Soman
-
Aby Abraham
Abstract
Some of the rapidly developing technologies in orthodontics are digital imaging, 3-dimensional modeling, and printing. 3-D printing uses a layer-by-layer manufacturing technique to create scaffolds that can be used for many applications. With the advent of digital surface imaging and 3-dimensional prototyping, new avenues for producing physical models have opened. The traditional clinical decision-making process has been revolutionized by the incorporation of 3-D printing which makes it convenient for clinicians to avoid physical model storage areas and better visualization of anatomical structures and treatment planning. This paper presents the advancements in additive manufacturing techniques for customized patient care in Orthodontics including recent advances in printing technology and materials. The potential application of 4D printing as an advanced manufacturing technology and the challenges and future perspectives for additive manufacturing are also highlighted.
Introduction
Contemporary orthodontists utilize the technologies available to overcome past communication barriers to optimize treatment plans, and patient care, and consequently increase the productivity. The orthodontist now has an arsenal of digital documentation at his disposal that facilitates orthodontic diagnosis, treatment planning, and treatment follow-up. Digital radiographs and digital photographs have replaced conventional methods of physical imaging, and concomitant cone beam computed tomography (CBCT) is being increasingly employed almost in every field of Orthodontics. Following this development, plaster models are now rapidly replaced by digital models and have several advantages such as accuracy and speed in obtaining data for diagnosis, no physical space needed for storage, the possibility of information transfer through a digital environment, easier orthodontic analysis, and the creation of virtual setups. An abundance of treatment options became available recently due to the increased number of technological innovations including advancements in orthodontic wires, bracket designs, and access to three-dimensional (3D) applications. One of the advantages of these innovations was the ability to treat the majority of orthodontic cases without extractions utilizing better diagnostic approaches and incorporating better materials and techniques in the treatment. A rapidly advancing digital technology in Orthodontics is 3-dimensional modeling and printing, making a transition from a traditional laboratory environment into a digital workstation. Recent advances in intraoral digital scanning technology have given orthodontists the ability to eliminate unpleasant impressions while providing patients with more accurate appliances and reduced treatment time. The next paradigm shift in orthodontics has evolved with the development of three-dimensional printers, working in conjunction with intraoral scanners.[1], [2], [3]
3D printing
3D printing is a method of conversion of digital files into three-dimensional solid objects using computer-aided software and 3D printers. It is also known as Additive manufacturing or Rapid prototyping. 3D printing is a technology whereby sequential layers of material are deposited on top of one another to eventually form an object. It is the opposite of subtractive manufacturing, in which a block of material is carved away to form the object (as with milling units such as CEREC). Three-dimensional (3-D) printing applications in orthodontics have made the treatment procedures easy, time-saving, and cost-effective. [1]
History
The concept of 3D printing was first developed by Charles (Chuck) Hull in 1984; using ultraviolet light to cure tabletop coatings which he called Stereolithography (SLA).In the year 1988, Hull established the 3D Systems Company to market the first commercial product, the SLA1. [1] In 1988, Scott Crump developed fused deposition modeling (FDM), which was commercialized by Stratasys in 1990. In 1993, the Massachusetts Institute of Technology (MIT) patented "3-D Printing techniques" similar to the inkjet technology used in 2D Printers.[2] Objet Geometries, the developer of PolyJet photopolymer (PPP) printing, was founded in 1998. In 2015, De Simone and co-workers reported a new generation of 3D printing method and apparatus, known as CLIP (Continuous Liquid Interface Production). [4]
Procedures in 3D Printing
The 3D printing process usually begins with a 3D model, virtually designed or obtained through scanning of a physical object. Slicing software automatically transforms the point cloud into a stereolithographic file which is sent to the additive manufacturing machine for building the object. The steps involved in the process of 3-D printing are as follows.
Digital scanning
Processing digital model
3D model printing
Digital Scanning
Digital cast models can be produced either by direct or indirect techniques. The direct method uses intraoral scanners and the indirect method uses either laser scanning or computed tomography imaging of the impression or plaster models. Subsequently, the scans are converted into digital images that are stored on the manufacturer's server. [5], [6]
Processing digital model
An intraoral scanner is used to create a digital file of the object in Standard Tessellation Language(STL), which was initially invented by Chuck Hull, the global format for 3D printing files. Computer-aided design and manufacturing (CAD/CAM) software is used to further process the file and prepare it for printing. [7] The STL file is perhaps the single most important item in the 3D printing workflow. Its simplicity creates some drawbacks like describing only surface geometry, no representation of color, and the items can be printed in just a single color. In addition, STL does not provide copyright information, file security, or the ability to detect errors in the surface mesh. Another open file format is PLY, a polygon file format (also known as Stanford triangle format), which is used when color and/or transparency information is needed. [8]
3D model printing
Additive technologies
Currently, there is a huge selection of 3D printing technologies suitable for orthodontic use, and the various technologies, applications, advantages, and limitations are shown in Table.I
Stereolithography:
SLA is a method and apparatus that uses a movable photon source to activate photopolymerization of the photocurable resin and successively print solid layers one on top of the other. After being built, objects are immersed in a solvent bath for excess resin removal and are consequently placed in a UV oven to finish the curing process. Based on object complexity and size, stereolithography can take from a few hours to more than 24 hours to create a particular part.
Fused deposition modeling:
It is the most commonly used 3D printing technology. Here, instead of curing a liquid resin with projected light, an FDM printer extrudes a resin that has been heated just beyond its melting point, depositing it layer by layer. The heated material hardens immediately after being extruded, thus minimizing inaccuracies.
Digital light processing:
DLP is identical to SLA except for the light source in which a projector is used to cure an entire layer at a time in contrast to the SLA laser, which must draw the entire layer to cure it, this results in significantly faster print time. The heart of the DLP projector is a chip known as a digital micromirror device, and the chip contains thousands of tiny mirrors that can move in two directions, on and off, thousands of times per second. Because a DLP printer builds a model in voxels rather than layers, there are no visible steps, making the finish quality the best of all 3D printing technologies.
PolyJet photopolymerization:
It employs the same basic technology as the standard inkjet office printer but in three dimensions. A liquid resin is jetted out of hundreds of nozzles and immediately cured with ultraviolet light. The build platform moves vertically to accommodate subsequent layers. The surface quality of PPP models is often excellent. Higher-end PPP printers can print multiple materials on a single model. There is typically more waste with PPP printers than with other technologies because a wiping blade is used before curing each layer to remove excess material and ensure dimensional accuracy. [1]
Selective laser sintering
This technology utilizes high-density lasers having superior printing quality applicable in dental implants, printed metal frameworks, and restorations. Though the technique involves higher operational and material costs, their applications are more biocompatible and require fewer patient appointments thereby enhancing patient comfort. [9]
Computed axial lithography
Printing around an object was one of the drawbacks with many conventional techniques like SLA and DLP and layer-by-layer addition of material could be possible with this new technique. It was invented by rotating a photopolymerizable material in a dynamically evolving light field. The technique suits high-viscosity photopolymers and multi-material production.
Melt electrowriting
This is another manufacturing process combining the molten polymer extrusion printing technique and the electrospinning concept, where an electrical field is continuously applied to the extruder. The fiber diameter range goes from ~ 2–50 μm and can reach the nanometric scale field depending on the polymer and the printing parameters. Those sizes are significantly thinner than FDM scaffolds, and the technique presents better control over the deposition when compared to conventional electrospinning, which contributes to guiding cell fate in tissue regeneration strategies.
|
S.No. |
3D Printing technique |
Applications |
Advantage/Limitation |
|
1. |
Stereolithography (SLA) |
Customized printed models, implant/surgical guides, templates, aligners & scaffolds |
Advantage: High resolution, high clinical accuracy & suitable for fabrication of patient specific devices Limitations: High cost,weak mechanical properties & material toxicity |
|
2. |
Fused Deposition Modeling (FDM) |
Surgical splints, guides for plates and mini screws, metal frame works in customized expansion devices and retainers in cleft palate patients. |
Advantage: High mechanical strength and porosity due to mechanical lay down. Limitation: Lack of ability to form complex structures and anatomical structures with complex shapes. For manufacturing a clean product, hollow internal structures or blind-ended openings are especially troublesome |
|
3. |
Digital Light Processing (DLP) |
Patient-specific models, implantable devices, fixed and removable prostheses devices, temporary restorations, implant/surgical guides, templates, crowns, custom trays, and scaffolds |
Advantages: high resolution and high clinical accuracy, suitable for manufacturing highly accurate patient-specific devices due to its design flexibility, and ability in geometrical scaling and shaping. Limitations: high cost, limited number of resins available, weak mechanical properties, potential material toxicity |
|
4. |
Polyjet Photopolymerization (PPP) |
Printed models, aligners, retainers and other orthodontic appliances |
Greater surface finish & ability to print multiple materials on a single model |
|
5. |
Selective Laser Sintering (SLS) |
Implant placement, printed metal frame works in maxillary expansion and cleft palate care. |
Advantage: More biocompatible and fewer patient appointment Limitations: High operational and material cost. |
|
6. |
Computed Axial Lithography (CAL) |
Customization of dental crowns, prosthetic devices, and possible printing of tissue, and coating of the devices |
Possibility to print around pre-existing objects and to manufacture objects with higher complexity and better surface finish in a shorter time |
|
7. |
Melt Electrowriting (MEW) |
Tissue engineered scaffolds for craniofacial structures and membranes for periodontal regeneration |
Advantage: High resolution & optimal to produce tissue scaffolds Limitation: High cost & complex system |
3D Printers Used in Orthodontics
The typical two-dimensional printer used for printing on paper works along the right-to-left x-axis and the top-to-bottom y-axis. In 3D printing, the up-and-down z-axis is added. MakerBot and Objet are the 3D printers recently acquired by Stratasys and currently used in dentistry and Orthodontics. The details of some of the currently used 3-D printers and their application are given in Table.II
Objet30 OrthoDesk
Objet30 OrthoDesk (Stratasys, Ltd., Eden Prairie, MN) employs the PolyJet printing technology and is suitable for orthodontic offices and small to medium-sized orthodontic labs. The build area for the OrthoDesk is 300mm × 200mm × 100 mm, which allows as many as 12 horseshoe-shaped models to be printed in a single job. It can print at 9mm (vertical height) per hour and three materials are used with this technology, Vero DentPlus (MED690), Clear biocompatible (MED610), and VeroGlaze(MED620).
Ultra 3SP Ortho
The Ultra 3SP Ortho printer was designed specifically for dental use and employs the Scan, Spin, and Selectively Photocure (3SP™) technology, a DLP variant, which utilizes a laser diode with an orthogonal mirror spinning at 20,000 rpm. The printer can produce highly accurate and stable dental models that could be used for orthodontic appliance fabrication. The models are resistant to high temperatures and have negligible water absorption. The build tray measures 266mm × 178mm × 76mm. This technology provides significantly faster print times: a maximum rate of 10mm per hour. Materials used with the Ultra 3SP Ortho are E-Denstone, the most popular medium for orthodontic use; ABS 3SP White, an ABS-like plastic; and E-Glass, a new, clear medium that can be used for a variety of applications.
MakerBot and other FDM printers
FDM models are generally the least expensive of the 3D printers, the materials are significantly less expensive as well which is one-third of the cost of material for Stratasys or EnvisionTEC printers. These were designed for hobbyists and not for the rigorous usage of an orthodontic office, reliability could also be an issue.
|
Technique |
Objet Eden 260VS |
Ultra® 3sp™ |
MakerBot Replicator 2 |
Formiga P 110 |
|
Company |
Stratasys, Ltd., Eden Prairie, Minn. |
EnvisionTEC, Gladbeck, |
Stratasys, Ltd., Eden Prairie, Minn. |
Eos, Munich, Germany |
|
Technology |
PolyJet Printing Technology |
Digital Light Processing |
Fused Depositing Modelling |
Selective Laser Sintering |
|
Materials |
A Variety Of Photopolymers |
Resins For Photopolym-erization |
Polylactic Acid(PLA), Acrylonitrile Butadiene Styrene (ABS), Polycarbonate (PC), Polyether Ether Ketone (PEEK) etc. |
Powders such as Alumide, Polyamide, Glass-Particle Filled Polyamide, Rubber Like Polyurethane etc. |
|
Applications |
High Quality Orthodontic Models |
Orthodontic Appliances |
Retainers And Aligners With Less Esthetic Appearance Due To Stair-Stepping |
High Quality Retainers And Orthodontic Appliances |
Materials Used in 3-D Printing
Print medium or materials are available as either unwound from a spool, dispensed from a sealed container or poured from a container into a vat. The print medium may be any of the several materials, including plastic, metal, clay, sand, and even human cells, each of which is best suited to a specific type of printer. Materials used for specific printers are as follows:
SLA- UDMA (Urethane Dimethacrylate
FDM - The most common are polylactic acid and acrylonitrile butadiene styrene (ABS
PolyJet printer: Materials specially engineered for dentistry are:
Clear Bio-compatible (MED610): Can produce orthodontic appliances, Delivery and positioning trays, and surgical guides for orthognathic surgery.
Vero Dent Plus (MED690): A dark beige material that creates amazingly fine features and finish, and offers excellent strength, accuracy, and durability placement.
Vero Glaze (MED620): An opaque material with A2 shading designed to provide a suitable color match for veneer try-ins and diagnostic wax-ups. Vero Glaze is medically approved for temporary in-mouth placement, for up to 24 hours.
Ultra 3SP Ortho
Press-E-Cast (WIC300)
Denstone (HTM140 Peach) - a peach color material able to achieve the look and feel of traditional gypsum models with a high-accuracy detail.
D3 White- a fast-growing, tough material with similar characteristics to ABS plastic and the most common medium for dental model manufacturing for the production of orthodontic appliances
Application in Orthodontics
Attempts are made to build dental models, removable appliances, customized brackets and archwires, and occlusal splints. Currently, the most common applications of the 3D printers are for clear retainers and aligner fabrication, appliance fabrication, 3D study models, fabrication of customized fixed appliance attachments and auxiliaries, fabrication of customized surgical guides and splints in orthognathic surgery and cleft lip and palate care.
Clear aligner fabrication
Clear aligner therapy involves a series of minor tooth movements achieved through the application of a corresponding series of individual aligners, which are changed in sequence throughout treatment. The Invisalign® system and comparable clear aligner systems generally involve digital manipulation of a digital impression of the dentition of the patient to develop a series of small sequential tooth movements from the initial condition to the desired final outcome. [7], [8], [9], [10] Physical models of the arches corresponding with each step then are fabricated via 3D printing for the fabrication of thermoforming aligners. [11] ([Figure 1]). Many factors may influence the efficiency of the workflow and the dimensional fidelity of the printed part:
Print layer height selection.
Digital model orientation concerning the printer platform and design of supporting structures.
Print layout.
Design of the model (shape of base, hollowing of interior of models). [12], [13], [14]
Printed model production typically involves post-print processing steps before the application of the model in thermoforming clear aligners.
Direct appliance printing
Skipping the step of 3D printing a physical model, researchers have also used the technology to digitally design a retainer and consequently 3D print it in a fine polyamide material. The direct printed appliances now popularly used are bite guard, printed lingual retainers, direct printed aligners, traction devices for canine impaction and rapid expanders made with an EnvisionTEC printer. As printing technology and materials improved, however, orthodontists could be able to design and fabricate brackets, auxiliaries, expanders, retainers, and aligners directly from a 3D printer, without the need for physical models. [15]
3-D study models
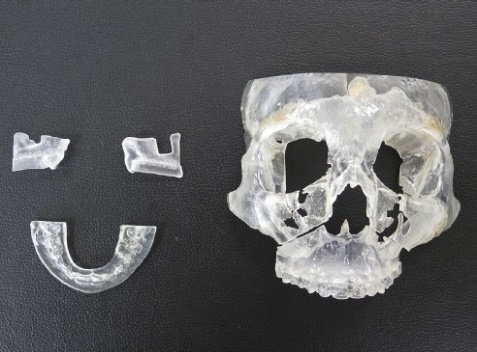
One of the rapidly developing areas in digital technology is three-dimensional modeling which uses intra-oral scanned data to create digital models. The advantages of digital models include no physical storage requirement, instant accessibility, ability to do digital diagnostic or treatment simulations, positive patient perceptions, ability to immediately send to an outside laboratory, no risk of breakage, wear, degradation, or loss, and an overall improved continuity of care; in addition, digital models are less labor intensive. Physical replicas of digital models can be obtained by 3-D printing and is the most common prototyping which is an advantage in orthodontic treatment planning ([Figure 2]). Two common methods of 3-D printing available now are Digital Light Processing (DLP) and PolyJet printing which uses additive manufacturing to fabricate a model. Both the DLP and polyJet printers produce clinically acceptable models with high accuracy that may allow them to serve as a replacement for stone models and to be considered viable options for clinical applications. Studies documented that the polyJet printer produces models with clinically acceptable accuracy for all recorded measurements. Compared with the DLP printer, the polyJet produced models with closer accuracy to the stone models. [16]
Customization of orthodontic treatment
This entails the use of two or more appliance systems during orthodontic treatment. Designing and printing custom fixed appliances involves establishing the "wire plane", and customization of the bracket with the use of a 3D-printed custom base and connector. It is then applied to the patient using the bracket transfer system [17], [18] An essential part of quality in orthodontic treatment is the standard production of archwires. Rapid development in 3D printing technology has led to the design and production of customized archwire models which have demonstrated uniform distribution of dentofacial stress, improved patient wearing comfort, and decreased tooth repair and treatment time. [19]
Custom-made brackets
Orthodontic treatment with fixed appliances is conventionally made by pre-programmed metallic or non-metallic brackets which have many drawbacks like lack of adaptation to the tooth surface, positioning difficulties due to abnormal size of the tooth, and difficulty in expression of first, second, and third order compensations. Custom-made brackets using computer technology have resolved this problem by obtaining digital images of teeth and supporting tissues and virtual models of brackets created by 3-D printing technology. After segmentation of the malocclusion on the model generated by intra-oral scan data, brackets can be digitally placed on the teeth and a target occlusion can be created. This defined tooth position can be used as a template to generate an individualized arch form in the horizontal plane. The base contour of the bracket can also be matched with the shape of the tooth surface with a positioning guide which is pre-fabricated to ensure that the bracket is bonded in the correct position and angulation. The arch wires can be constructed according to the template and individually pre-bend to meet the requirement. [18]
The effectiveness of these custom-made brackets with conventional direct and indirect bonding has been tested. They concluded that custom-made brackets manufactured by CAD-CAM technology were found to be effective in treatment outcomes about treatment time and fewer archwire changes compared to standard brackets. [20] A standardized technique based on individual 3D design and heat pressing to produce printed customized esthetic ceramic brackets from lithium disilicate material has evolved and proven to be highly efficient. [21] In lingual orthodontics, the HIRO system was modified with a 3D printer to align teeth three-dimensionally into their desired final position and to fabricate a final printed model on which lingual brackets were positioned, which was tested clinically and found to be a viable option. [22]
Orthodontic auxiliaries
With the new generation printers rendering accurate, affordable, and instant prototypes, 3-D printing has proven to be efficient in orthodontic practice when compared with the fabrication of attachments by conventional methods like injection molding. Many orthodontic auxiliaries can be designed with modeling software that slices the digital model into thousands of virtual layers and translates the data into a numerical controlled programming language called G-code. The specifications are then sent to a stereolithographic (SLA) or fused deposition modeling (FDM) printer which forms the fabrication of auxiliary layer by layer from a plastic filament or resin material. Retraction hooks, lingual retainers, and aligner attachments can be made of SLA printing technology and turbo bites can be fabricated by FDM technology. [23]
Orthognathic surgery
The development of 3-D printed models and patient-specific guides has improved surgical planning and transfer of surgical plans into the operating room for a better surgical outcome. In general, the clinical application of this technology in orthognathic surgery includes the production of occlusal splints, osteotomy cutting guides, repositioning guides, custom-made fixation plates, and 3-D printed models.
Surgical splint fabrication
Computer-assisted orthognathic surgery has gained popularity in recent years, as the technologies offer improved possibilities for pre-operative planning, surgical transfer, and quality control of the procedure. In conventional orthognathic surgery, pre-operative model surgery followed by the fabrication of more than one surgical splint to precisely position the segments was the gold standard. Fabrication of this splint is time-consuming and errors associated with positioning are a common problem. Precise surgical splints could be produced by computer-assisted technology and later a pre-operative preparation of surgical splints for orthognathic surgery by 3-D printing has been introduced. [24], [25], [26] Evidence suggests that the surgical splints made with conventional methods using models and computer-assisted technology are proved to be equivalent for routine clinical use, and the computer-assisted surgical splints are efficient in reducing the time and effort required for surgical planning. [27], [28]
Osteotomy guides and repositioning guides
Osteotomy guides are useful in placing the surgical cuts exactly as in digital planning so that repositioning guides can place the surgical segments in the desired position. They provide a reliable, innovative, and precise approach for translation of the virtual plan to the operating room ([Figure 3]). Computer-designed genioplasty guides, guides fitted on the mandibular incisor for genioplasty and chin templates were introduced first to transfer the osteotomy line and the planned position of chin. [29], [30], [31], [32], [33], [34] Osteotomy involving the maxilla and mandible can also be planned specifically using cutting guides and 3-D printed patient-specific fixating plates (PSI) for accurate final positioning of jaws greatly reducing human errors. Intraoperative 3-D printed surgical splints are also an option to position jaws where patient-specific fixation plates are not an option. [35]
Fixation plates and implants
Patient-specific fixation plates are planned based on accurate 3-D imaging and can fix the osteotomy segments into the correct position. Patient-specific titanium plates fabricated by using the EOS Titanium Ti64 system (Electro Optical Systems) for maxilla segment repositioning and fixation without the use of surgical splints. [35], [36] Many studies documented that these titanium implants provide precise positioning and fixation as well as adequate stability of Le Fort I osteotomy of maxilla. [37]
3-D printed surgical models
Fabrication of 3-D models from computer-generated images has greatly improved the surgical outcome in many orthognathic surgery cases through precise pre-operative assessment, surgical planning, intra-operative orientation, and pre-bending of mini plates for fixation ([Figure 4]). Many of the drawbacks of conventional surgery like inaccuracies in segment positioning and abnormal condylar positioning or sag can be avoided by this novel method of model fabrication. [38] Common technologies for the fabrication of 3-D printing models are Selective Laser Sintering (SLS), Three Dimensional Printing(3DPTM), and PolyJetTM.




Cleft lip and palate
Nasoalveolar moulding
Conventional presurgical nasoalveolar molding has been used traditionally to treat maxillary alveolar defects in newborn babies with cleft lip and palate. The main drawbacks of this procedure are frequent visits and trimming of acrylic as the segment approximates and the chances of dislodgement of the appliance when it exerts pressure on the nasal tips using stents. To reduce these problems, virtual models can be taken the proposed final alveolar position is designed and a series of molding devices are fabricated using 3-D printing technology. [39]
Surgical Simulators
Surgical simulators are emerged as one of the training tools in contemporary trainee education. They provide real-life standardized, safe, and competency-based surgical education for anatomic structures that lack cadaveric availability. In cleft lip surgical repair, this tool is found to be very effective especially when the surgery is performed in very young children where this pediatric procedure learning is difficult. Virtual reality-based cleft lip surgical repair educational devices which are 3-D printed using computer graphics with real-time haptic feedback are found to be effective in teaching programs of cleft lip repair ([Figure 5]). This model may accelerate and enhance trainee exposure to the execution of this advanced procedure. The use of readily available materials, compatibility with standard surgical equipment, and the reusable-replaceable modular design result in a relatively low overall cost, making it accessible to many training environments in the future. [40]
Patient education and surgical training models
Many cases of cleft management involve education about the deformity involved to the patient and parent and an explanation about the planned interventions and potential outcomes. Traditionally, pre-operative and post-operative treatment photographs, study models, and radiographs were used for this purpose. Though two-dimensional models were found to be effective in providing a more physical evaluation of the cleft area, digital surface imaging and 3-D prototyping of the affected area opened new avenues in physical evaluation. For patients consulting for cleft-related speech problems or in preparation for alveolar bone grafting, the models allow the clinician to easily describe the anatomic challenges of the problem under consideration. The sagittal view of the model is particularly useful in demonstrating the concepts of the velopharyngeal port, and it shortens the amount of time needed to describe the anatomy to the parent. These 3D models for use in education are printable with additive manufacturing technology are made from multiple materials, and can be utilized to demonstrate a large spectrum of clinical issues related to cleft conditions. [41]
Maxillary protraction using 3-D printed plates
Skeletal class III malocclusions with deficient maxilla can be effectively moved forward by the application of orthopedic force in young adolescent children. The main drawback of this procedure is unwanted tipping of anteriors and extrusion of posterior teeth, especially molars. Force application through mini plates can minimize these drawbacks and enhance the skeletal movement of the maxilla. Root position of posteriors, buccal cortical plate thickness, and adaptation of mini plates are some of the usual problems encountered with this protocol. A customized design with 3-D printed titanium plates has been introduced for effective maxillary protraction.[42] The production of surgical guides using 3D printing technologies is increasingly becoming popular since it provides a simple and safe method of inserting mini-implants, with customized adaption, precision, and accuracy for both miniplate and mini-screw placements, maximum surface contact between miniplate/mini-screw and bone, and lower failure rates of mini-screws. [43] Based on CBCT images, the morphology of the maxillary and infra zygomatic region can be visualized and the plates can be adapted well and positioned using surgical guides.
4D printing
One of the emerging trends in this technology is incorporating stimuli-responsive materials that can perform a pre-determined function. It adds time as a new dimension to the 3D printing technology that performs functionally as desired in response to stimuli. The materials used can adapt, sense, and be responsive which perform multifunctionally. [44] It has wide applications in the medical and dental field especially in implantology and maxillofacial surgery as surgical guides. Regarding this, titanium implants might be replaced with shape memory materials to enhance implant biocompatibility and osteointegration. These shape memory polymer materials have many applications in orthodontics including bite rising in deep bite correction, arch expansion, and also evoke cellular response against mechanical stimuli in orthodontic tooth movement. [45]
Discussion
3D printing and additive manufacturing is one of the technological advancements in the specialty of Orthodontics which revolutionized contemporary diagnosis and appliance fabrication. Over the years, many technological advancements in this new area have evolved to produce more precision, accuracy, printing materials, and time. Most of the studies on orthodontic models revealed that the printed models are accurate and suitable for clinical use. [46], [47] The methods used for 3D printing documented that both SLA and Polyjet printing are accurate and precise for model fabrication and SLA printing had higher precision than Polyjet printing. [41] Kim et al evaluated the precision and accuracy of DLP, SLA, FFF, and Polyjet printing and found that models printed with DLP and Polyjet printing were more accurate than SLA and FFF methods. [48]
To overcome the geometric inaccuracies in aligner fabrication due to the heat forming process when a thermoforming material is vacuum formed, various developments in aligner materials have evolved.3D printed aligners were compared with thermoform aligners vacuum formed from 3D printed models showed that the geometric accuracy was increased in 3D printed aligners11. Thermoplastic materials such as Duran and Durasoft for the vacuum forming technique and dental LT Resin for direct 3D printing were compared for compatibility and bite force and showed that dental LT Resin was a superior material for aligners. Biocompatibility of the materials was evaluated between dental LT Resin, E-Guard, and SmartTrack which showed that SmartTrack was considered to be the least cytotoxic material. [49]
Newly printed bone scaffolds revolutionized the 3D printing technology, especially in knee replacement and craniofacial deformities. This development promises a huge leap in the management of craniofacial pathologies and orthognathic surgeries in the future. They can serve as a learning tool for training and mock surgery before the actual surgeries so that the risks and complications can be evaluated. From additive-manufactured surgical templates, autotransplantation, and bioprinted scaffolds the new phase of reconstructive modalities is impressive and efficient.
Though the future of 3D printing is promising, some of the concerns and challenges regarding this excellent technology should not be overlooked. The cost of 3D printers, the biodegradability of the materials, and their influence on the ecosystem have to be well studied. The printer running time, maintenance, material cost, need for skilled operators, and adherence to strict health and safety protocols are carefully considered. From a regulatory perspective, the printing materials must meet the required standards for dental application in terms of bioactivity and technical aspects. It is important to conduct extensive cytotoxicity and biocompatibility studies before releasing 3D printing materials to be used in the body. The selection of materials and post-processing techniques is integral to creating a high-quality product with minimal adverse effects on the human body. Choosing aligners from reputable manufacturers adhering to good manufacturing practices, coupled with patient-specific considerations and close dental supervision are crucial for mitigating risks and ensuring safe and effective treatment. [50]
Conclusion
With the addition of 3-D printers, Orthodontists can achieve a complete digital workflow for increased treatment efficiency. Eliminating the traditional impressions and stone models not only reduces clutter and storage requirements in the office, but enhances practice efficiency, improves appliance fit, allows model reuse, and results in improved treatment outcomes. This new technology brings the specialists a novel way of imaging, diagnosing, documenting, and communicating with the patient and a referral system for efficient patient management and delivery of quality care. It provides information helpful for clinicians and researchers considering the use in clinical aspects particularly in decision making. The application of this new technology should be explored further in various other areas as well as research work in the future.
Source of Funding
None.
Conflict of Interest
None.
References
- Groth C, Kravitz N, Jones P, Graham J, Redmond W. Three-dimensional printing technology. J Clin Orthod. 2014;48(8):475-85. [Google Scholar]
- Mahamood S, Khader M, Ali H. Applications of 3-D Printing in Orthodontics: A Review. Int J Sci Study. 2016;3(11):267-70. [Google Scholar]
- Groth C, Kravitz N, Jeffrey M. Incorporating three-dimensional printing in orthodontics. J. Clin. Orthod. 2018;52(1):28-33. [Google Scholar]
- Bagheri A, Jin J. Photopolymerization in 3D Printing. ACS Appl Polym Mater. 2019;1:593-611. [Google Scholar]
- Westerlund A, Tancredi W, Ransjö M, Bresin A, Psonis S, Torgersson O. Digital casts in orthodontics: A comparison of 4 software systems. Am J Orthod Dentofacial Orthop. 2015;147(4):509-16. [Google Scholar]
- Hazeveld A, JHS, Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am J Orthod Dentofacial Orthop. 2014;145(1):108-15. [Google Scholar]
- Hennessy J, Al-Awadhi E. Clear aligners generations and orthodontic tooth movement. J Orthod. 2016;43(1):68-76. [Google Scholar]
- Kravitz N, Groth C, Shannon T. CAD/CAM software for three-dimensional printing. J Clin Orthod. 2018;52(1):22-7. [Google Scholar]
- Lin L, Fang Y, Liao Y, Chen G, Gao C, Zhu P. 3D Printing and Digital Processing Techniques in Dentistry: A Review of Literature. Adv Eng Mater. 2019;21(6). [Google Scholar] [Crossref]
- Melkos A. Advances in digital technology and orthodontics: a reference to the Invisalign method. Med Sci Monit. 2005;11(5):39-42. [Google Scholar]
- Jindal P, Juneja M, Siena FL, Bajaj D, Breedon P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am J Orthod Dentofacial Orthop. 2019;156(5):694-701. [Google Scholar]
- Loflin W, English J, Borders C, Harris L, Moon A, Holland J. Effect of print layer height on the assessment of 3D-printed models. Am J Orthod Dentofacial Orthop. 2019;156(2):283-9. [Google Scholar]
- Zhang Z, Li P, Chu F, Shen G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J Orofac Orthop. 2019;80(4):194-204. [Google Scholar]
- Short M, Favero C, English J, Kasper F. Impact of orientation on dimensional accuracy of 3D-printed orthodontic models. J Clin Orthod. 2018;52(1):13-20. [Google Scholar]
- Nasef A, El-Beialy A, Mostafa Y. Virtual techniques for designing and fabricating a retainer. Am J Orthod Dentofacial Orthop. 2014;146(3):394-8. [Google Scholar]
- GB, Currier G, Kadioglu O, Kierl J. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am J Orthod Dentofacial Orthop. 2018;154(5):733-9. [Google Scholar]
- Krey K, Darkazanly N, Kühnert R, Ruge S. 3D-printed orthodontic brackets - proof of concept. Int J Comput Dent. 2016;19(4):351-62. [Google Scholar]
- Wiechmann D, Rummel V, Thalheim A, Simon J, Wiechmann L. Customized brackets and archwires for lingual orthodontic treatment. Am J Orthod Dentofacial Orthop. 2003;124(5):593-9. [Google Scholar]
- Liu G, Qin H, Zhen H, Liu B, Wang X, Tao X. 3D printing of personalized archwire groove model for orthodontics: design and implementation. Int J Adv Comput Sci Appl. 2018;9(12). [Google Scholar] [Crossref]
- Brown MW, Korluk L, Ko CC, Zhang K. Effectiveness and efficiency of CAD/CAM orthodontic bracket system. Am J Orthod Dentofacial Orthop. 2015;148(6):1067-74. [Google Scholar]
- Yang L, Yin G, Liao X, Yin X, Ye N. A novel customized ceramic bracket for esthetic orthodontics: in vitro study. Prog Orthod. 2019;20(1). [Google Scholar] [Crossref]
- Kara-Boulad J, Burhan A, Hajeer M, Khattab T, Nawaya F, RA. Treatment of moderately crowded teeth using lingual fixed appliance prepared by a modified HIRO® technique: a case report and method description. Cureus. 2022;14(5). [Google Scholar] [Crossref]
- SA, Kanna AA, Kumar RV. 3D-printed orthodontic auxiliaries. J Clin Orthod. 2015;5:217-21. [Google Scholar]
- Mortadi NA, Eggbeer D, Lewis J, Williams R. CAD/CAM/AM applications in the manufacture of dental appliances. Am J Orthod Dentofacial Orthop. 2012;142(5):727-33. [Google Scholar]
- Metzger M, Hohlweg-Majert B, Schwarz U, Teschner M, Hammer B, Schmelzeisen R. Manufacturing splints for orthognathic surgery using a three-dimensional printer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):1-7. [Google Scholar]
- Lauren M, Mcintyre F. A new computer-assisted method for design and fabrication of occlusal splints. Am J Orthod Dentofacial Orthop. 2008;133(4):130-5. [Google Scholar]
- Gateno J, Xia J, Teichgraeber J, Rosen A, Hultgren B, Vadnais T. The precision of computer-generated surgical splints. J Oral Maxillofac Surg. 2003;61(7):814-7. [Google Scholar]
- Adolphs N, Liu W, Keeve E, Hoffmeister B. RapidSplint: virtual splint generation for orthognathic surgery - results of a pilot series. Comput Aided Surg. 2014;19(1-3):20-8. [Google Scholar]
- Olszewski R, Tranduy K, Reychler H. Innovative procedure for computer assisted genioplasty: three dimensional cephalometry, rapid prototyping model and surgical splint. Int J Oral Maxillofac Surg. 2010;39(7):721-4. [Google Scholar]
- Olszewski R, Szymor P, Kozakiewicz M. Accuracy of three dimensional, paper based models generated using a low cost, three dimensional printer. J Craniomaxillofac Surg. 2014;42(8):1847-52. [Google Scholar]
- Kang S, Lee J, Lim S, Kim Y, Kim M. Validation of mandibular genioplasty using a stereolithographic surgical guide: in vitro comparison with a manual measurement method based on preoperative surgical simulation. J Oral Maxillofac Surg. 2014;72(10):2032-42. [Google Scholar]
- Lim S, Kim M, Kang S. Genioplasty using a simple CAD/CAM (computer-aided design and computer-aided manufacturing) surgical guide. Maxillofac Plast Reconstr Surg. 2015;37(1). [Google Scholar] [Crossref]
- Li B, Shen S, Yu H, Li J, Xia J, Wang X. A new design of CAD/CAM surgical template system for two piece narrowing genioplasty. Int J Oral Maxillofac Surg. 2016;45(5):560-6. [Google Scholar]
- Yamauchi K, Yamaguchi Y, Katoh H, TT. Tooth bone CAD/CAM surgical guide for genioplasty. Br J Oral Maxillofac Surg. 2016;54(10):1134-35. [Google Scholar]
- Mazzoni S, Bianchi A, Schiariti G, Badiali G, Marchetti C. Computer-aided design and computer-aided manufacturing cutting guides and customized titanium plates are useful in upper maxilla waferless repositioning. J Oral Maxillofac Surg. 2015;73(4):701-7. [Google Scholar]
- Suojanen J, Leikola J, Stoor P. The use of patient_specific implants in orthognathic surgery: a series of 32 maxillary osteotomy patients. J Craniomaxillofac Surg. 2016;44(12):1913-6. [Google Scholar]
- Huang S, Lo L, Lin C. Biomechanical optimization of a custom - made positioning and fixing bone plate for Le Fort I osteotomy by finite element analysis. Comput Biol Med. 2016;68:49-56. [Google Scholar] [Crossref]
- Ibrahim D, Broilo T, Heitz C, Oliveira MD, Oliveira HD, Nobre S. Dimensional error of selective laser sintering, three_dimensional printing and PolyJet models in the reproduction of mandibular anatomy. J Craniomaxillofac Surg. 2009;37(3):167-73. [Google Scholar]
- Zheng J, He H, Kuang W, Yuan W. Pre-surgical nasoalveolar moulding with 3-D printing for a patient with unilateral cleft lip, alveolus and palate. Am J Orthod Dentofacial Orthop. 2019;156(3):412-9. [Google Scholar]
- Reighard C, Green K, Rooney D, Zopf D. Development of a Novel, Low-Cost, High-fidelity Cleft Lip Repair Surgical Simulator Using Computer-Aided Design and 3-Dimensional Printing. JAMA Facial Plast Surg. 2019;21(1):77-9. [Google Scholar]
- Chou P, Hallac R, Shih E, Trieu J, Penumatcha A, Das P. 3D-Printed Models of Cleft Lip and Palate for Surgical Training and Patient Education. Cleft Pal Craniofac J. 2018;55(3):323-7. [Google Scholar]
- Shuran L, Fan W, ZD. Preliminary application of three-dimensional printing titanium plate anchoring anterior traction for the treatment of skeletal class III malfarmatios. Chin J Stomatol. 2017;52(12):753-5. [Google Scholar]
- Cantarella D, Quinzi V, Karanxha L, Zanata P, Savio G, Fabbro MD. Digital workflow for 3D design and additive manufacturing of a new miniscrewsupported appliance for orthodontic tooth movement. Appl Sci. 2021;11(3). [Google Scholar] [Crossref]
- Chen X, Han S, Wu W, Wu Z, Yuan Y, Wu J. Harnessing 4D printing bioscaffolds for advanced orthopedics. Small. 2022;18(36). [Google Scholar] [Crossref]
- Sharma D, Mathur VP, Satapathy BK. Biodegradable and biocompatible 3D constructs for dental applications: Manufacturing options and perspectives. Ann Biomed Eng. 2021;49:2030-56. [Google Scholar]
- Dietrich C, Ender A, Baumgartner S, Mehl A. A validation study of reconstructed rapid prototyping models produced by two technologies. Angle Orthod. 2017;87(5):782-7. [Google Scholar]
- Koretsi V, Kirschbauer C, Proff P, Kirschneck C. Reliability and intraexaminer agreement of orthodontic model analysis with a digital caliper on plaster and printed dental models. Clin Oral Investig. 2019;23(8):3387-96. [Google Scholar]
- Kim S, Shin Y, Jung H, Hwang C, Baik H, Cha J. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am J Orthod Dentofacial Orthop. 2018;153(1):144-53. [Google Scholar]
- Ahamed S, Kumar S, Vijayakumar R, Kanna AA, KID. Apros Kanna AS, Indrapriya dharshini K. Cytotoxic evaluation of directly 3D printed aligners and Invisalign. Eur J Mol Clin Med. 2020;7(5):1141-9. [Google Scholar]
- Jeng J, Wang F, Wu S, Chang C, Liu W. Biocompatibility and Potential Cytotoxicity of 3D-Printed Dental Materials: A Review. Int J Mol Sci. 2022;23. [Google Scholar]
- Abstract
- Introduction
- History
- Procedures in 3D Printing
- 3D Printers Used in Orthodontics
- Materials Used in 3-D Printing
- Application in Orthodontics
- Clear aligner fabrication
- Direct appliance printing
- 3-D study models
- Customization of orthodontic treatment
- Orthognathic surgery
- Surgical splint fabrication
- Osteotomy guides and repositioning guides
- Fixation plates and implants
- 3-D printed surgical models
- Cleft lip and palate
- Maxillary protraction using 3-D printed plates
- 4D printing
- Discussion
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Kumar GS, Dharshini CP, Soman PS, Abraham A. 3D printing – A paradigm shift in orthodontic appliances and patient care [Internet]. J Dent Panacea. 2024 [cited 2025 Nov 07];6(4):171-180. Available from: https://doi.org/10.18231/j.jdp.2024.035
APA
Kumar, G. S., Dharshini, C. P., Soman, P. S., Abraham, A. (2024). 3D printing – A paradigm shift in orthodontic appliances and patient care. J Dent Panacea, 6(4), 171-180. https://doi.org/10.18231/j.jdp.2024.035
MLA
Kumar, G Sreejith, Dharshini, C Priya, Soman, Prasanth Soni, Abraham, Aby. "3D printing – A paradigm shift in orthodontic appliances and patient care." J Dent Panacea, vol. 6, no. 4, 2024, pp. 171-180. https://doi.org/10.18231/j.jdp.2024.035
Chicago
Kumar, G. S., Dharshini, C. P., Soman, P. S., Abraham, A.. "3D printing – A paradigm shift in orthodontic appliances and patient care." J Dent Panacea 6, no. 4 (2024): 171-180. https://doi.org/10.18231/j.jdp.2024.035
