Introduction
Eruption guidance in mixed dentition refers to the strategic management and intervention during the transition from primary teeth to permanent teeth, so as to ensure proper alignment and occlusion. This period typically occurs between the ages of 6 & 12 years and is crucial for establishing a healthy, functional and aesthetically pleasing dental arch.
An abnormal eruption of a tooth in an incorrect position in the dental arch is referred as ectopic eruption. The eruption anomalies are classified as position-related disorders (ectopic eruption and transpositions) and timing related disorders (premature eruption, delayed eruption or impaction).1 Nikiforuk defined ectopic eruption as “a condition in which the permanent teeth, because of deficiency of growth in the jaw or segment of jaw, assume a path of eruption that intercepts a primary tooth, causes its premature loss and produces a consequent malposition of the permanent tooth”.2 There can be various reasons for teeth to erupt ectopically, such as genetic factors, trauma (injury to the primary teeth), space constraints, pathological conditions (presence of cysts/ tumors) and abnormal tooth anatomy.
Early detection and intervention are pivotal to effectively manage ectopic eruptions, as untreated cases can lead to complications including malocclusion, cyst formation, and even resorption of the adjacent teeth. Besides, abnormal eruption may increase the risk of dental caries and periodontal problems if the teeth are in harder-to-clean areas.
The maxillary central incisors are crucial for both function and aesthetics in the dental arch, as they are the most visible teeth when smiling, speaking, and interacting socially; their proper alignment improves appearance and boosts self-confidence. Additionally, their correct position in the dental arch ensures effective biting and chewing while playing a vital role in articulating sounds such as “s” and “th”.
Interceptive orthodontic intervention helps to manage the ectopic eruption and correction of teeth alignment. There are various approaches which could be followed that depends mainly on the severity of the displacement, the age of the patient and the specific tooth involved. It is a multistep process that requires careful planning & co-ordination among dental professionals. Also, regular follow ups and a tailored treatment plan are essential for achieving the best outcomes. In this case report, we describe the management of an ectopically erupted maxillary permanent right central incisor.
Case Report
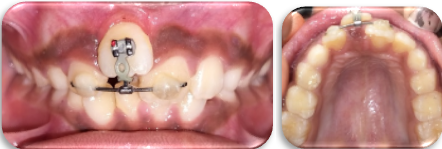
A healthy 9-year-old patient had visited the department of pediatric and preventive dentistry, P.M.N.M Dental College and Hospital, Bagalkot with the chief complaint of irregularly arranged teeth in the upper front region. No significant medical or habitual history was noted, but the parents reported a history of delayed exfoliation of a deciduous tooth in the same region, which was extracted at a private dental clinic 3 months ago. (Figure 1, Figure 3)
Upon intraoral examination, the patient was found to be in the early mixed dentition stage, with Angle’s class 1 molar relation bilaterally and a fair oral hygiene. Her maxillary right central incisor had erupted ectopically, positioned high in the labial sulcus, resulting in an overjet measuring 9 millimetres w.r.t tooth 11. (Figure 2, Figure 4) Further intra-arch examination revealed that her teeth were non-carious, although there was crowding observed in the mandibular anterior region. (Figure 5)
Treatment plan
Moyer’s mixed dentition analysis indicated that the space available is greater than the space required to accommodate the erupting permanent teeth. However, it is important to note that Moyer's analysis may lead to over- or underestimation of values, particularly in the Indian population, as it is not fully accurate or calibrated for this demographic.
The initial treatment planning comprised of 2 stages:
The “SPA” Approach
For facilitating controlled movement of 11, a specialized orthodontic traction appliance was designed called as the SPA appliance. The components were
MBT Bracket (slot size 0.022 inches) for the tooth 11
An 18*25 Rectangular NiTi wire
A short crimpable hook
Chain elastics
Red orthodontic elastics
After performing oral prophylaxis, an MBT bracket (pre-adjusted edgewise bracket of slot size 0.022 inches) was carefully bonded onto the labial aspect of tooth 11. Afterwards, the 18*25 rectangular NiTi wire was cut and contoured accordingly and was bonded to 21 to 12 using the composite and wire splinting technique. A short crimpable hook was attached to the centre of wire and chain elastic was engaged from the hook to the bracket of 11.
Before engaging the elastic, the crimpable hook was firmly secured. A short elastomeric chain was cut to the appropriate length, ensuring proper engagement from the hook to the bracket. Using a Mathew plier, one end of the chain elastic was carefully stretched and hooked around the crimpable hook, ensuring it was securely placed to prevent slippage during function. The other end of the chain was extended to the bracket and wrapped around it. The chain elastic was checked to ensure it provided the correct amount of tension for the intended tooth movement—neither too tight, which could cause excessive pressure, nor too loose, which would render it ineffective. The force exerted by the elastics on the tooth was maintained at 50 grams. After engagement from the hook to the bracket, the chain's positioning and patient comfort were verified. (Figure 6) Then, the patient was instructed to maintain proper oral hygiene and to do tooth brushing with caution so that the elastic won’t get dislodged from the hook.
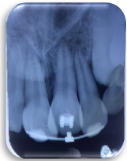
During the patient's follow-up appointment, conducted 15 days later, positive results were observed, including significant orthodontic movement of tooth 11 in both the incisal and palatal directions, as well as improved upper lip support. (Figure 7) In the next visit, in an effort to improve the traction force (60 grams), the chain elastic was replaced with a red orthodontic elastic. (Figure 8) Radiographical evaluation was conducted with respect to tooth 11, which showed sufficient bone support and no signs of root resorption. (Figure 9) Within one month of treatment, notable improvements were observed: the pre-operative overjet of 9mm, was reduced to 6mm, and the distance between the incisal edges of 11 and 21 reduced from 8.5mm to 6.5mm (measured using digital vernier calliper). This proved the efficacy of the new traction appliance in the treatment of ectopically erupted incisor.
In the fourth visit, the treatment plan was advanced with the initiation of 2x4 appliance therapy, which involved bonding MBT brackets to the upper central and lateral incisors, as well as molar tubes to both upper first permanent molars, and engaging a 0.012 NiTi arch wire. (Figure 10) After 2 weeks, the arch wire was changed to 0.014 NiTi wire. (Figure 11) The alignment of 11 was achieved within 2 weeks of wire change and the appliance was debonded and a removable thermoform retainer (2 mm thickness) was delivered to prevent relapse. (Figure 12, Figure 13)
Discussion
Tooth eruption refers to the process by which a tooth moves from its initial formation (developmental) position within the jaw to its final, functional placement in the dental arch. Ectopic eruption is defined as a condition in which the tooth follows an improper path of eruption, deviating from its usual course, often resulting in the tooth appearing in an unexpected location in the mouth. The order of ectopic eruption observed is mandibular lateral incisors > maxillary central incisors > maxillary canines > maxillary lateral incisors > mandibular central incisors > maxillary first molar > mandibular canines > mandibular first molar.3 Also ectopically erupted tooth may result in midline shift,4 root resorption of adjacent teeth, 5 may lead to infection, cyst formation, 6 abnormal growth of jaw, loss of arch length, and abnormal relationship with opposing dentition. 7
These variation in the normal eruption patterns of maxillary incisors are common in children. Due to the prominent location of these teeth, parents often become concerned when the eruption does not follow typical patterns and they seek treatment to prevent any psychological impact associated with it.
Ectopic eruption is prevalent in almost 5.6% of general population and majority of cases reported showed the involvement of permanent central incisors. The incisors are reported to erupt ectopically or seen as impacted due to supernumerary tooth in about 2% of population. 8, 9 Ectopic eruption, typically unilateral in the maxillary incisors, 8 occurs more frequently in girls,9 however, Huber et al. found no significant correlation between sex and the incidence frequency of ectopic eruptions. 8
In the present case, retained deciduous tooth was the cause for ectopic eruption of the respective permanent tooth. Barberia et al. reported that the ectopically erupted tooth corrected itself spontaneously after the removal of the etiological agent. 10 Huber et al. suggested extracting the corresponding primary incisor to allow for natural guidance of ectopically erupted teeth in cases where the deviation is minimal. 8 Suresh et al. reported two cases of retained primary incisors with ectopically erupting central incisors unilaterally. In these cases, self-correction occurred within three months after the removal of the etiological agent. They also described a case of an ectopically erupting central incisor due to an interfering mesiodens, where self-correction did not occur. For this case, the authors used a 2×2 Begg's appliance to align the ectopically erupting tooth after the mesiodens was removed. 9 Ebru et al. reported a case of an ectopically erupting maxillary central incisor caused by an intrusive injury to the predecessor tooth where they used a combination of fixed and removable orthodontic appliances to align the tooth. 11 Jacob c et al. reported a case of ectopic eruption of maxillary central incisors due to retained primary incisors bilaterally. Here, fixed orthodontic treatment using a 2×2 appliance was opted following the extraction of retained primary incisors. 12
When abnormally positioned ectopically erupted incisors are moved into the arch, discrepancies are often observed between the gingival levels of the affected and neighbouring teeth. 11 Clinical experience has shown that light forces are more effective than strong ones in moving ectopically erupted teeth and achieving a good gingival position. 13
In the current case, a novel approach on orthodontic traction appliance was taken by designing the “SPA” approach, instead of directly opting for fixed orthodontic therapy. The components used in this appliance require only less chair side time and is extremely well tolerated by the patient. Orthodontic elastics were placed from the bracket of tooth 11 to the crimpable hook attached to the splinted rectangular NiTi wire running from tooth 12 to tooth 21. The slow and continuous force applied through the elastics facilitated a more controlled tooth movement. The appliance proved its efficacy in reducing the overjet by correcting the increased palatal root torque. Another significant benefit of this new appliance is that it does not interfere with the patient’s ability to maintain proper oral hygiene. This fresh perspective on treating the ectopically erupted incisor reduced the risk of incisal flaring due to minimal anchorage and thereby the complexity & treatment duration of 2 * 4 appliance.
Conclusion
Treatment of the ectopically erupted incisors in early mixed dentition are often challenging due to its abnormal position and the insufficient arch length. However, newer alternative strategies must be attempted in intercepting this malocclusion in children. The 'SPA' appliance that is debuted in the present case has established its efficacy to address such misalignments in an easier and versatile manner.