Introduction
Peripheral ossifying fibroma (POF) is a non-neoplastic growth, which occurs on the gingiva in response to trauma or irritation. It is a reactive lesion of connective tissue.1 It is believed to comprise about 9% of all gingival growths. Trauma and local irritants such as plaque, calculus, micro-organisms, masticatory forces, ill-fitting dentures and poor quality restorations are considered as etiology of peripheral ossifying fibroma. Though the etiopathogenesis is undefined, an origin from cells of the periodontal ligament has been suggested.2 POF may also develop as a maturation of a pre-existing pyogenic granuloma or peripheral giant cell granuloma.3 POF is also described as peripheral cementifying fibroma, peripheral odontogenic fibroma, and peripheral fibroma with calcification. The lesion appears as a slow growing solitary mass which is usually sessile with a smooth or ulcerated surface. It tends to occur in the 2 and 3 decades of life. Females are more commonly affected than males with difference of 66% in females. It affects maxilla more than mandible with anterior region being the common site of occurrence of POF. An important clinical aspect of POF is the high recurrence rate is estimated from 8% to 45%.4 Surgical excision is the treatment of choice for POF. The lesions like POF have been treated with scalpel surgery, electrocautery & laser.5 Laser provides advantages over scalpel method such as bloodless surgical field, minimal damage to adjacent tissue and little or no scar formation.
The present paper reports the successful management and 1-year follow‑up of POF treated with hard & soft tissue laser Er: YAG.
Case Report
A 48 years female patient reported to department of Periodontics with a chief complaint of swelling in left palatal region of jaw. Intraoral examination revealed an approximately 2.5*1.5 cm, pedunculated, pale pink growth present on the palatal aspect in relation to the left premolar-molar region. It was non-tender on palpation. The growth was firm in consistency.[Figure 1] CBCT was taken which showed calcification present palatally in 16 region.[Figure 2] Patient was systemically healthy. There was no history of trauma. A provisional diagnosis as peripheral ossifying fibroma was given. Differential diagnosis as pyogenic granuloma, peripheral giant cell granuloma was given.
Surgical procedure
Scaling and root planing was performed. Oral hygiene instructions were given. Excision of lesion was planned using Er: YAG laser. Informed consent was taken from the patient. The area was anesthetized with adequate local anaesthesia (Lignocaine with adrenaline). A traction suture was given near to the base of lesion.[Figure 3] Tip diameter of 0.8mm was used soft tissue excision in contact mode and hard tissue removal and smoothening was done at no-contact mode.[Figure 4] Complete excision of lesion was done[Figure 5] and given for histopathological report. Complete hemostasis was achieved. [Figure 6] Periodontal dressing was placed. Post-operative instruction & analgesic and antibiotic were given.[Figure 7]
Histological examination
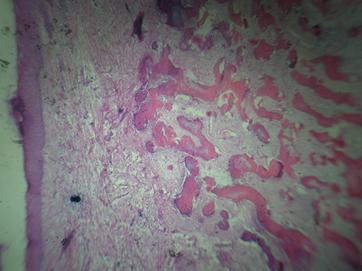
Histological examination showed a parakeratinized stratified squamous epithelium. Underlying connective tissue was highly cellular with a large number of fibroblasts. Areas of calcification were also seen. Presence of cellular connective tissue and foci of bone in the histological picture confirmed the diagnosis of POF. [Figure 8]
Discussion
Gingiva shows wide variety of lesions occurring ranging from inflammatory to neoplastic.6 Eversole and Rovin in 1972 described POF as a reactive lesion of gingiva. The term Peripheral ossifying fibroma was given by Gardner in 1982.7 The histogenesis of POF is still unknown. POF can occur as an inflammatory hyperplasia of cells of the periodontal ligament. Metaplasia of the connective tissue can be seen as dystrophic calcification.8 Or it may initially develop as a pyogenic granuloma, which then undergoes fibrous maturation and calcification.9
POF has female predilection and the anterior maxilla is the common site of occurrence. POFs can occur at any age, with a peak in the second decade of life.10 In these case POF present in female patient in the palatal region.
Clinically POF has to be differentiated from other reactive lesions. Most of the lesions are difficult to differentiate clinically. They can be differentiated histologically. Pyogenic granuloma exhibits vascular proliferation similar to granulation tissue. PGCG is characterized by scattered giant cells within a fibrous stroma. Peripheral odontogenic fibroma in histological examination contains islands of odontogenic epithelium.8
In majority of cases there is no underlying bone involvement which is visible on the radiograph. Sometimes, there may be superficial erosion of bone.11
Histologically, POF shows fibrous proliferation and the formation of mineralized components.12 Various components are seen in POF: i) Dystrophic calcifications, ii) Bone (woven/lamellar), iii) Cementum.13
One challenging aspect of surgically treating POF is its recurrence rate, which has been reported to vary from 7% to 45%. The high recurrence rates of lesion is attributed to the surgical technique and its thoroughness. A superficial removal and curettage is more likely to result in a recurrent lesion. A thorough debridement is essential to prevent recurrence. Excision of lesion using laser provides advantages over other surgical instruments including, a dry and bloodless surgery, sterilization of the surgical site, reduced mechanical trauma, minimal scarring, and wound contraction accelerating recovery and post‑operative function.14 We have used Er: YAG laser for excision. The laser of the erbium family shows higher water absorption coefficient leading to rapid vaporization and micro explosions that creates high pressure on the surrounding cells.15 Advantages of Er:YAG laser are: less thermal damage to adjacent tissue, generates reactive oxygen species(ROS) causing sterilization of field, minimum carbonization, causes expression of collagen & elastic fibres thus promoting wound healing.