- Visibility 115 Views
- Downloads 13 Downloads
- DOI 10.18231/j.jdp.2024.043
-
CrossMark
- Citation
Prosthodontic management of orbital defect using custom-made eye shell- A case report
Introduction
Most orbital abnormalities result from treating cancers that originate in the orbital contents, or from tumors spreading to the palate, nasal cavity, paranasal sinus, skin surrounding the tumor, and intraoral mucosa.
Significant facial deformity, functional difficulties, and adverse psychological effects are caused by these anomalies in patients. The purpose of reconstruction is to:
Create a distinct opening between the nasal and oral cavities; and enable normal breathing without obstruction.
To achieve visually acceptable results.
An alternative to surgical reconstruction is prosthetic rehabilitation. These prosthetics offer a respectable aesthetic appearance and replicate the patient's missing structures. They also allow for the monitoring of the defect for tumor recurrence and the maintenance of cleanliness around it.[1]
Terminology
Orbital exenteration
This is the removal of the orbital fat, periorbita, eyelids, extraocular muscles, and eyelashes in their entirety or in part.
Orbital enucleation
This is the process of removing the globe by cutting the optic nerve and extraocular muscles, together with its contents, the cornea, and the sclera. The orbital muscles remain intact and the periorbital fat, eyelids, lashes, and surrounding bones are left undisturbed by orbital enucleation.
Orbital evisceration
This procedure involves extracting the globe's contents (uvea), potentially including the cornea, while maintaining the sclera's integrity and connection to the extraocular muscles. Additionally, it preserves the optic nerve. [2]
Definition
According to glossary of prosthodontic terms -10
Ocular prosthesis
It is defined as a maxillofacial prosthesis that artificially replaces an eye missing as a result of trauma, surgery, or congenital absence; the prosthesis does not replace missing eyelids or adjacent skin, mucosa or muscle. [3]
Orbital prosthesis
It is defined as a maxillofacial prosthesis that artificially restores the eye, eyelids, and adjacent hard and soft tissues. [3]
Classification systems
Kesting classification (2017): [4]
Defects were divided into four groups by their system, with A and B subtypes found in the second category.
Type 1: Simple orbital exenteration with an intact bony orbit is included in the defect.
Type 2a: Orbital exenteration and the loss of a single orbital wall are examples of defects.
Type 2b: Multiple orbital wall loss is one of the defects.
Type 3: Orbital exenterations with faults in the skull base are described by deficiencies.
Type 4: Extended exenterations with a piercing orbitomaxillary defect are among the faults.
Locoregional flaps can be used to successfully restore Type 1 and 2a/b defects, but vascularized free flap reconstruction is necessary for higher grade lesions.
Cinar et al classification: [5]
Defects are classified by their system into kinds 0 through 4, with subtypes A and B.
Type 0: Indicates a defect with fully intact bony orbital walls; these defects can be repaired using a variety of techniques, such as free skin grafts, vascularized flaps (free or pedestaled), or secondary intention healing therapy.
Type 1: Defines a defect where the orbital floor and/or medial orbital wall are penetrated by a sinonasal fistula.
Type 2: When the dura is intact, flaws are characterized by cranio-orbital fistulas caused by deficiencies in the superior orbital bone. Restoring the distance between the orbit and the cranial vault in these anomalies is essential to reducing the risk of meningitis, encephalitis, and other complications. flaps with vascularization, either pedicled (such as a temporalis flap) or free (such as a radial forearm free flap), are necessary to recreate the barrier.
Type 3: Defects lack entire dura but resemble type 2 bony defects.
Type 4: Cranio-orbito-nasal fistulas are the defects.
With the exception of type 0, all deformities can also be categorized as subtype A or subtype B depending on whether a maxillectomy with preserved palate or a complete maxillectomy is used. Locoregional flaps, in general, are frequently used for reconstruction of types 1 and 2, whereas types 3 and 4 often require one or multiple vascularized free flaps.
Modes of retention of orbital prosthesis:
Adhesive, straps, spectacle frames, and implants are among the different methods of retention. [6]
Eye glasses
By using specially made eyeglass frames, patients may be able to keep their nasal, ear, or ocular prosthesis. Rather than being translucent, the color of the eyeglass frame should be opaque to hide retention marks.
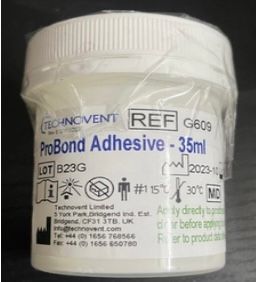
Adhesives
Adhesive ideal specifications for maxillofacial prosthesis. [7]
It need to adhere well to the prosthetic and facial skin.
Adhesive biocompatibility.
The patient's skin texture.
The patient's ease of handling the adhesive.
Examples of its composition include polyethylene oxide, karaya gum, tragacanth, sodium carboxyl methyl cellulose, flavorings, and antimicrobials.
Benefits
Economicalness
Non-interference
Absence of harmful side effects
Drawbacks
During insertion and removal, it may cause harm to the skin as well as the prosthesis's surface.
May result in dermatitis in touch.
Is able to change the prosthesis' color.
Adhesives may erode and disturb the prosthesis structure. [7], [8]
Implants
An additional implant or two was frequently inserted in the inferior orbital rim or zygoma.[9]
An implant can also be placed in the outer canthus, inner canthus, and superior orbital rim.
There should be no facial angling of the implant.[10]
To allow access for hygiene, implants typically have a length of 3–4 mm and a spacing between them of 10–12 mm.
Magnets are the retentive mechanisms with implants that are most frequently used. [11]
The typical healing time is six to eight months.
Orbital prosthesis implants come in the following types:
Non-integrated (such as silicone implants and PMMA)
Allen implants are semi-integrated.
Implants that are integrated (Cutler's implants).
Hydroxyapatite structures with or without integration porus polyethylene, with the prosthesis made of aluminum oxide, are examples of biointegrated materials.
Biogenic implants (grafting dermal fat onto the prosthesis to create cancelous bone). [12]
Case Report
Subject
Male (aged 36 years)
Referred to
Department of Prosthodontics
Chief complaint
Facial Disfigurement Due to Loss of the Left Eye.
Medical history
Exenteration of orbit (performed one year ago due to mucor-mycosis).
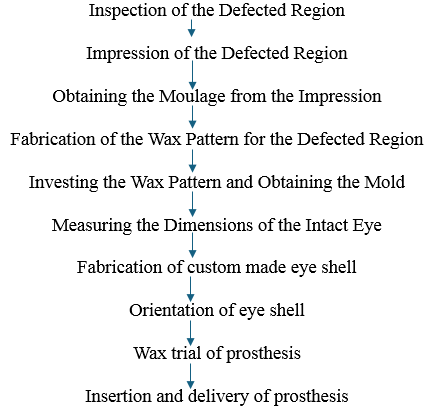
Procedure followed to fabricate orbital prosthesis
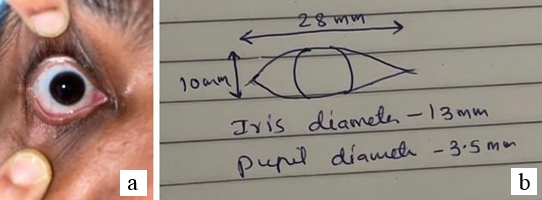
Following examination and assessment of the defect site and anophthalmic socket ([Figure 2]), the surrounding areas, including the lashes and eyebrows, were softly moistened with vaseline. Irreversible hydrocolloid imprint material, also known as alginate, is utilized to record the anopthalmic socket and is reinforced with dental plaster. The alginate impression material was stabilized using dental plaster ([Figure 3]). Using modeling wax, the finished impression was enclosed and the spaces were filled ([Figure 4]). Gypsum product type III was filled with cast. ([Figure 5]). For the purpose of creating a custom ocular prosthesis, a wax model ([Figure 6]) that resembled the shape of the globe was built. It was then filled with type III gypsum material and the mold was filled with acrylic resin. After the patient is fitted with the customized shell, the extensions are marked with a pencil and the excess is cut off ([Figure 7]). Using a scale and divider, the diameters of the pupil and iris on the intact side were measured ([Figure 8] a,b):
Iris Diameter --13 mm
Pupil Diameter -- 3.5 mm
Width of Sclera at Rest from Inner to Outer Canthus -- 28 mm
Height of Sclera from Eyelid to Eyelid at Central Region --10 mm
Height of Sclera at Retraction -- 13 mm.
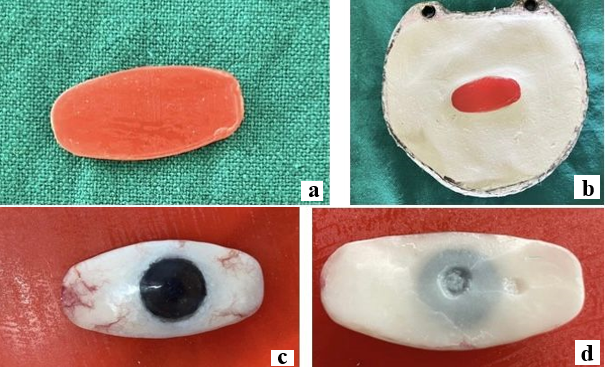
The dimensions of the undamaged eye were measured, and a wax pattern was created based on those measurements. The wax pattern was then invested in type II gypsum product ([Figure 9]a,b).
A disk of auto-polymerizing acrylic resin, about 1.0 mm thick and 1.0 mm in diameter less than the selected iris size, was created.
The disk was painted using acrylic-based pigments. The painted iris disk's color fidelity was compared to that of the human eye ([Figure 9]c,d).
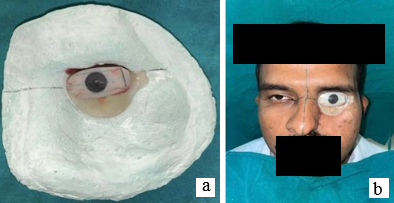
The prosthesis's flat area was painted the iris's base color, and the pupil was represented by a black dot. The assembly was tried in after an ocular button was luted to the ready flat surface ([Figure 10]a). As the patient gazed straight at the observer's eye, its orientation was changed ([Figure 10]b). In order to create the wax trail of the prosthesis ([Figure 11]a,b) and the eyelid aperture, two small wax strips were softened and placed over the ocular portion for the initial assessment. The prosthesis was treated using intrinsic coloring ([Figure 12]). Following the completion of the polymerization, an abrasive stone was used to finish the leftover flush, which had been cut back with a scalpel. Extrinsic staining was carried out chairside using an extrinsic staining kit because the patient's skin tone was not as dark as the prosthesis' color ([Figure 13]).










Post-operative considerations
An year follow-up is required to assess the orbital prosthesis, tissue bed, and look for tumor recurrence. [13] Every day, patients are instructed to take off and clean their orbital prosthetic. A glue-retained prosthesis's ability to integrate marginally can be lost due to deterioration and exposure to sunshine, air pollution, and color changes. A prosthesis should endure for at least one to five years, however other writers recommend replacing it after only six to nine months if the defect size or color changes. [14]
Discussion
An orbital prosthesis ought to be aesthetically pleasing, long-lasting, affordable, and, above all, retentive. The patient's aesthetic requirements, anatomical factors, economical considerations, etc., all influence the retention method and material selection for the orbital prosthesis.
Two materials that are frequently used to create orbital prostheses are silicone elastomers and acrylics. Rigidity is the main drawback of acrylic. [15] Silicone elastomers have the benefit of offering more lifelike translucency; nevertheless, their inability to connect chemically or mechanically with the eyeglass frames is a drawback.
Skin allergies are the main disadvantage of adhesive-retained prostheses. Since there was little anatomical undercut in this instance, the patient was advised to apply glue. The patient was at ease with the prosthesis, thus he did not need to wear glasses. [16]
Conclusion
For orbital prosthesis treatment, a multidisciplinary team approach and an appropriate reconstructive plan are essential. While implant-retained orbital prostheses are helpful in the effective treatment of orbital abnormalities, traditional adhesive-retained prostheses are more affordable, practical, and trouble-free. Wearing eyewear and adhesive together helps maintain the device in place. [16]
Source of Funding
None.
Conflict of Interest
None.
References
- B Shrestha, S Thaworanunta. Orbital prosthesis fabrication: current challenges and future aspects. Open Access Surg 2016. [Google Scholar] [Crossref]
- J Klimczak, S Helman, S Kadakia, R Sawhney, M Abraham, AK Vest. Prosthetics in facial reconstruction. Craniomaxillofac Trauma Reconstr 2018. [Google Scholar]
- . Glossary of prosthodontic terms. J Prosthet Dent 1977. [Google Scholar]
- MR Kesting, S Koerdt, N Rommel, T Mücke, KD Wolff, CP Nobis. Classification of orbital exenteration and reconstruction. J Craniomaxillofac Surg 2017. [Google Scholar]
- C Cinar, H Arslan, U A Bingol, Y Aydin, O Cetinkale. The New Anatomical Classification System for Orbital Exenteration Defect. J Craniofac Surg 2017. [Google Scholar]
- SA Nazar, VV Nair, KK Harsha, R Ravichandran. Retention in maxillofacial prosthetics: A review. Int J Appl Dent Sci 2021. [Google Scholar]
- R Saini, A Nagpal, K Thakur, R Saini, R Shrivastav. Retentive aids in maxillofacial prosthesis: A review . IP Ann Prosthod Restor Dent 2019. [Google Scholar]
- AD Turksayar, SA Saglam, AC Bulut. Retention systems used in maxillofacial prosthesis: A review. Niger J Clin Pract 2019. [Google Scholar]
- A Visser, G M Raghoebar, R P Van Oort, A Vissink. Fate of Implnt-retained Craniofacial Prosthesis: Life Span and Aftercare. Int J Oral Maxillofac Implants 2008. [Google Scholar]
- C Sabarigirinathan, K Vinayagavel, G Sriramaprabu, P Rupkumar, NS Meena, J.Baranikrishnan. Implants in Maxillofacial Prosthesis. J Sci 2015. [Google Scholar]
- T Saia, M Kheur. Maxillofacial Prosthesis: All Insight into Their Retention and Support. Int J Dent Pract Med Sci 2013. [Google Scholar]
- S Shah, Y Shah. . Implants in ophthalmology . [Google Scholar]
- JYS Yi, EJ Dierks, LM Over, MJ Hauck. Prosthetic reconstruction of the orbit/globe. Oral Maxillofac Surg Clin North Am 2012. [Google Scholar]
- S Jain, P Jain. Rehabilitation of orbital cavity after orbital exenteration using polymethyl methacrylate orbital prosthesis. J Indian Prosthodont Soc 2016. [Google Scholar]
- C Veerareddy, KC Nair, GR Reddy. Simplified technique for orbital prosthesis fabrication: A clinical report. J Prosthodont 2012. [Google Scholar]
- AB Kunturkar, V Chuske, SS Khavnekar, R Gandagule, KG Mante, PN Borikar. Orbital Prosthesis - A Case Report. Int J Sci Stud 2023. [Google Scholar]
